Prevention
Modern medicine is increasingly transitioning towards preventive care. This shift towards prevention has also been observed in breast cancer care in recent years, particularly with the discovery of the BRCA gene. Subsequently, multiple genes and risk factors have been identified. Depending on these factors, a personalized screening strategy can be chosen. Therefore, it is crucial to understand these genetic and risk factors.
Diagnosis
I was diagnosed with cancer ... This website serves as a portal designed to assist you and your loved ones in accessing personal information and finding solutions to your concerns.
The primary goal of this website is to offer guidance and support to patients as they navigate their journey toward recovery and improved quality of life. The "Diagnosis" section of our website is divided into two main categories. Firstly, under "Anatomy and Physiology," we provide fundamental knowledge about the breast. Secondly, in the "Tumors and Disorders" section, we delve deeper into various breast-related conditions.
Moreover, we aim to provide information to women who may be concerned about potential breast issues but are hesitant to seek immediate medical advice. Knowledge and information can often offer immediate reassurance if a woman is able to identify the issue herself and determine that no specific treatment is necessary. Conversely, we also strive to educate women who have received a diagnosis of a serious breast condition, such as breast cancer, and wish to approach their doctor well-informed and prepared.
Treatment
The treatment for breast cancer should immediately include a discussion about reconstruction. Our foundation has no greater goal than to raise awareness of this among patients and oncological surgeons. By making an informed decision beforehand, we avoid closing off options for later reconstruction while still considering the oncological aspect. Of course, survival is paramount, and the decision of the oncologic surgeon will always take precedence.
The "Reconstruction or not?" page contains all the information you can expect during an initial consultation before undergoing tumor removal. This page is comprehensive, and your plastic surgeon will only provide information relevant to your situation.
"Removing the tumor" details the surgical procedure itself. This is the most crucial operation because effective tumor removal remains paramount. We guide you through the various methods of removal, a decision often made by a multidisciplinary team comprising oncologists, radiologists, pathologists, radiotherapists, breast nurses, gynecologists, oncological surgeons, and plastic surgeons.
The "Breast Reconstruction" section includes information and illustrations of the different reconstruction options along with corresponding steps.
Revalidation
Those treated for cancer often need a long period to recover.
Cancer is a radical illness with a heavy treatment. Often, people have to deal with psychosocial and/or physical problems afterwards, such as stress, anxiety, extreme fatigue, painful joints, reduced fitness, lymphedema... This can have a major impact on general well-being.
There are rehabilitation programmes offered by most hospitals. We cover some of the major topics here.
Quality of life
Quality of life is a key factor in coping with breast cancer. Therefore, it is important to find coping mechanisms that work, which will be different from patient to patient. For some, it may be finding enjoyment in activities they engaged in prior to diagnosis, taking time for appreciating life and expressing gratitude, volunteering, physical exercise... Of prime importance, studies have shown that accepting the disease as a part of one’s life is a key to effective coping, as well as focusing on mental strength to allow the patient to move on with life. In this section we are addressing some topics that patients experience during and after treatment and we are providing information to address them.
Additional Surgery
After the actual breast reconstruction, some additional surgery is still required. Breast reconstruction usually requires three stages.
The breast mound is re-created using an implant or autologous tissue.
Six months later a second procedure may be performed to improve symmetry with the contralateral breast.
The final stage involves nipple reconstruction and tattooing of the areola. Sometimes the other areola is also tattooed to achieve a similar colour match on both sides.
Recreation of the breast mound
If the reconstruction is being performed using a tissue expander, the volume can be gradually adjusted by injecting saline through a small port in the implant. Once the desired volume is reached, the expander can be exchanged for a permanent silicone implant. However, once the permanent implant is in place no further corrections can be made. If the breast volume needs to be altered again, additional surgery is necessary.
Immediately after an autologous breast reconstruction, the shape of the breast may be less natural. Over the first several months, gravity will take affect and the appearance will improve.
The free flap transfer and initial shaping is just the first step in achieving a full and natural breast reconstruction. Following the principles of a sculptor, we try to create a breast in the first step that is slightly bigger than the desired volume and resembles the final result as close as possible. Obtaining a definite result in one procedure is impossible. As removing tissues is so much easier than adding, specific areas of the flap can be aspirated or resected during the second operation 6 months later. This will improve breast symmetry which is the final goal of the procedure. If more tissue is needed, the flap can be augmented by lipofilling in specific spots to improve the shape or throughout the flap if a pure volume augmentation is necessary. Augmentation by implants is possible as well but performed less and less as results of lipofilling become more predictable and successful.
Nipple reconstruction is performed by using the modified C-V flap. Scar revisions and adjustments to the borders of the footprint can easily be performed. During the second operation, the colateral breast can also be corrected in case of unilateral reconstruction.
Nipple Reconstruction
Nipple reconstruction can be performed using skin that is already present on the breast. Nipple reconstruction is performed once the reconstructed breast has achieved its final position on the chest wall and acceptable shape and volume symmetry has been obtained between both breasts.
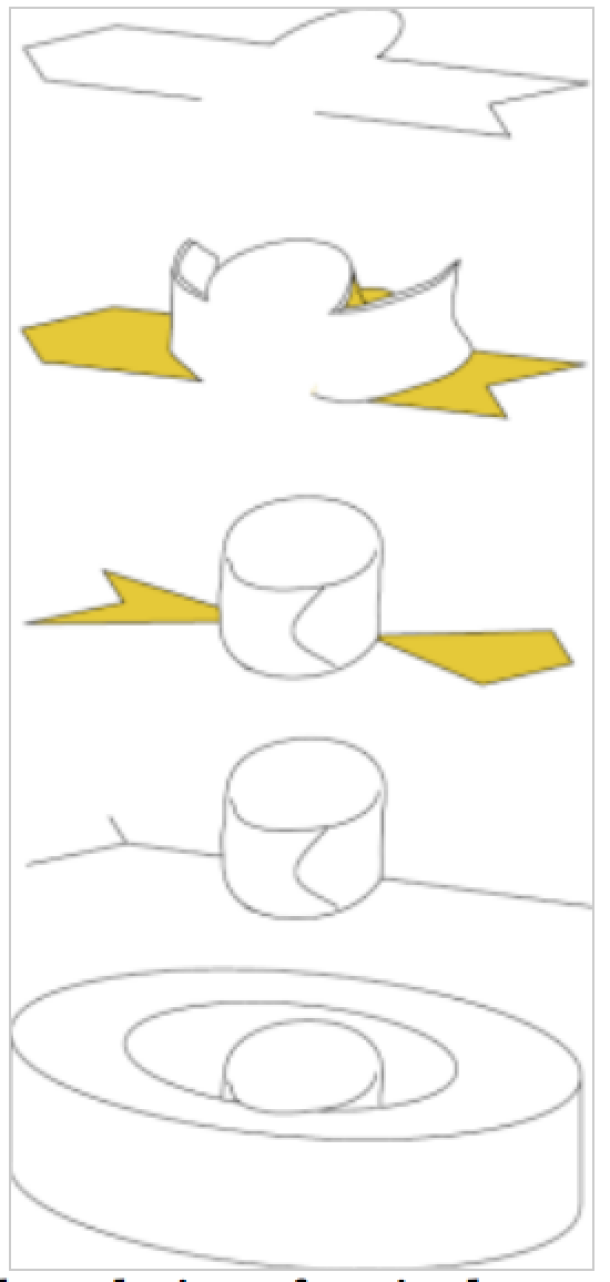
A clover-leaf pattern is designed, tilted and rotated (fig. 1). A small straight linear scar remains which can later be camouflaged by tattooing the pigmentation of the nipple-areolar complex. A protective, perforated dressing is positioned around the new nipple for a period of 4 weeks after surgery.
The restitution of the areola is done by tattoo only. The use of skin grafts coming from different areas of the body is no longer done. Tattooing is performed about 3 to 4 months after the last surgical procedure around the nipple. Tattooing of the areola is performed on both sides to guarantee the same color on both sides. Equal colors fool the eye and camouflage the “reconstruction-effect”.
Fig. 1 simple technique for nipple reconstruction |
Contralateral Breast
Some small adjustments may be necessary to the other breast. The aim is to achieve symmetry in both shape and volume. The decision on whether to perform surgery on the unaffected side is discussed with each patient at the start of the reconstructive process. During the first consultation, long term objectives are agreed. The patient is encouraged to comment on the unaffected side. If she is entirely satisfied with the shape and volume, then this breast serves as a model for the reconstruction.
If the patient is not satisfied with the unaffected breast, correction may be performed at a later stage. During the first procedure, an attempt is made to reconstruct a breast in keeping with the patient’s physique. At a second stage, the unaffected breast can be corrected so that both breasts are as symmetrical as possible. The reconstructed breast serves as a model for the unaffected breast.
Possible adjustments include breast augmentation, breast reduction or a breast lift. If there is an increased risk of breast cancer, a prophylactic mastectomy on the unaffected side may be considered and bilateral reconstruction offered as a simultaneous procedure.
References
Weelisch DK, Schain WS, Noone RB, Little JN. The psychological contribution of nipple addition in breast reconstruction. Plast Reconstr Surg. 1987;80:699-704.
Kroll SS, Reece GP, Miller MJ, et al. Comparison of nipple projection with the modified double-opposing tab and star flaps. Plast Reconstr Surg. 1997;99:1602-1605.
Anton MA, Eskenazi LB, Hartrampf CR Jr. Nipple reconstruction with local flaps: star and wrap flaps. Perspect Plast Surg. 1991; 5:67–78
Cronin ED, Humphreys DH, Ruiz-Razura A. Nipple reconstruction: The S flap. Plast Reconstr Surg. 1988;81:783–787.
Rubino C, Dessy LA, Posadinu A. A modified technique for nipple reconstruction: the ‘arrow flap’. Br J Plast Surg. 2003:56;(3):247–251.Losken A, Mackay GJ, Bostwick J III. Nipple reconstruction using the C-V flap technique: a long-term evaluation. Plast Reconstr Surg. 2001;108:361-369.
Shestak KC, Gabriel A, Landecker A; et al. Assestment of long-term nipple projection: a comparison of three techniques. Plast Reconstr Surg. 2002;110:457-463.
