Prevention
Modern medicine is increasingly transitioning towards preventive care. This shift towards prevention has also been observed in breast cancer care in recent years, particularly with the discovery of the BRCA gene. Subsequently, multiple genes and risk factors have been identified. Depending on these factors, a personalized screening strategy can be chosen. Therefore, it is crucial to understand these genetic and risk factors.
Diagnosis
I was diagnosed with cancer ... This website serves as a portal designed to assist you and your loved ones in accessing personal information and finding solutions to your concerns.
The primary goal of this website is to offer guidance and support to patients as they navigate their journey toward recovery and improved quality of life. The "Diagnosis" section of our website is divided into two main categories. Firstly, under "Anatomy and Physiology," we provide fundamental knowledge about the breast. Secondly, in the "Tumors and Disorders" section, we delve deeper into various breast-related conditions.
Moreover, we aim to provide information to women who may be concerned about potential breast issues but are hesitant to seek immediate medical advice. Knowledge and information can often offer immediate reassurance if a woman is able to identify the issue herself and determine that no specific treatment is necessary. Conversely, we also strive to educate women who have received a diagnosis of a serious breast condition, such as breast cancer, and wish to approach their doctor well-informed and prepared.
Treatment
The treatment for breast cancer should immediately include a discussion about reconstruction. Our foundation has no greater goal than to raise awareness of this among patients and oncological surgeons. By making an informed decision beforehand, we avoid closing off options for later reconstruction while still considering the oncological aspect. Of course, survival is paramount, and the decision of the oncologic surgeon will always take precedence.
The "Reconstruction or not?" page contains all the information you can expect during an initial consultation before undergoing tumor removal. This page is comprehensive, and your plastic surgeon will only provide information relevant to your situation.
"Removing the tumor" details the surgical procedure itself. This is the most crucial operation because effective tumor removal remains paramount. We guide you through the various methods of removal, a decision often made by a multidisciplinary team comprising oncologists, radiologists, pathologists, radiotherapists, breast nurses, gynecologists, oncological surgeons, and plastic surgeons.
The "Breast Reconstruction" section includes information and illustrations of the different reconstruction options along with corresponding steps.
Revalidation
Those treated for cancer often need a long period to recover.
Cancer is a radical illness with a heavy treatment. Often, people have to deal with psychosocial and/or physical problems afterwards, such as stress, anxiety, extreme fatigue, painful joints, reduced fitness, lymphedema... This can have a major impact on general well-being.
There are rehabilitation programmes offered by most hospitals. We cover some of the major topics here.
Quality of life
Quality of life is a key factor in coping with breast cancer. Therefore, it is important to find coping mechanisms that work, which will be different from patient to patient. For some, it may be finding enjoyment in activities they engaged in prior to diagnosis, taking time for appreciating life and expressing gratitude, volunteering, physical exercise... Of prime importance, studies have shown that accepting the disease as a part of one’s life is a key to effective coping, as well as focusing on mental strength to allow the patient to move on with life. In this section we are addressing some topics that patients experience during and after treatment and we are providing information to address them.
More breast surgery
I. Aesthetic Breast Surgery
A. Preoperative Stages
The Pre-Operative Consultation
For most plastic surgery procedures it is advisable to have two consultations with your surgeon. These are elective procedures, so there is no urgent medical need for the operation. Unlike emergencies such as appendicitis, it is the patient, not the doctor who determines when and by whom the surgery will be performed. Therefore it is imperative that the surgeon outlines all the possible approaches to your needs and their potential complications.
To have sufficient time to consider this information, a patient should therefore usually be offered two consultations. A few weeks between visits allow ‘cooling down’ time, to give the surgeon’s suggestions due consideration.
To best address your needs, it is essential that you inform the surgeon of your complete medical history, including:
all medications currently taken, especially those which may affect blood clotting
any significant past medical history
previous operations
allergies, including to drugs, sticky tapes or latex
Doing everything that you can to optimize your physical condition prior to surgery will also help to minimize the risk of complications. In particular, smoking increases the risk of:
Infection
Bleeding
Healing problems
Blood clots
Stopping even a few weeks prior to the procedure will improve this situation.
During the consultation the surgeon will emphasize his/her commitment to you, but also reiterate a patient’s obligation to themselves. This includes maintaining your health and availing yourself of all available information about the procedure from websites, literature and support groups. The surgeon may also have the contact details of previous patients who are happy to talk to you about their experiences of the operation and recovery. It may also be helpful to obtain a second opinion from another surgeon. It is, however, important to remember that different surgeons have different approaches to the same problem and sometimes too much advice can lead to confusion.
Between the Consultations and Surgery
Once the decision has been made to go ahead with surgery, your doctor will decide which preoperative health checks are necessary. Below is a list of frequently performed investigations, although not all people need all of these:
Blood tests for anaemia and clotting
Electrocardiogram (ECG) to check for heart conditions
Chest x-ray to check for lung problems
Mammography to check for early tumours
CT scanning to check previous health problems or for preoperative mapping of the blood supply to tissue
A plan will be made for any post-operative support garments that may be required such as bras or abdominal supports.
In the weeks before your surgery it is a good idea to prepare a bag, packed with all of the things you may need, including a sports bra as recommended by your surgeon. You will need to stop taking blood-thinning medicines like aspirin a week in advance and it is a good idea to reduce your intake of vitamin E and garlic. In some cases you may be advised to take a mild laxative or fibre supplement to minimise the risk of constipation, which can be a troublesome side-effect of many of the pain medicines used around the time of surgery.
At home it is wise to prepare for your return from surgery by having good supplies of easy-to-prepare meals or home help. Also ensure that you have enough of your normal prescription medication to last for 2 weeks following the procedure.
The night before surgery you must not eat or drink after midnight and definitely avoid alcohol.
Admission for Surgery
For large operations you may be asked to come in the night before, but for most procedures, arriving on the day of surgery is sufficient. Because your surgeon wants to ensure that all of the patients are properly prepared before starting to operate, he/she will usually ask everyone to arrive first thing in the morning. Those who are scheduled for surgery later in the day will need to have something to do, such as a good book but also a good deal of patience!
Your surgeon will visit you and answer any last minute questions before often taking photographs for your medical records. He/she will then make some pen drawings to plan the surgery with you in an upright position, as the shape of things changes when you lie down. This planning can still be rechecked during surgery using a tilting operating table.
B. Breast Augmentation
Description of the Problem
Breast augmentation is performed for women who feel that their breasts are too small (hypoplastic). In most cases there is only a need for additional volume but sometimes a mild droop can be completely corrected by the addition of an implant.
After liposuction, breast augmentation is the procedure most frequently performed by plastic surgeons.
If a breast is small and there is a significant droop, it may be necessary to carry out a breast lift at the same time as the augmentation. Then, both the form and the volume can be addressed.
When discussing the problems and solutions for breast hypoplasia, it is important to realise that the final result is significantly affected by the quality of the overlying skin and consistency of the breast tissue. The better the skin and the thicker the underlying subcutaneous fat, the more coverage of the implant and the more natural the result will be.
Aim of the operation
The goal is to increase the volume of the breast and/or to tighten the overlying skin. If a lift is also performed, the nipple will be moved upwards to a more aesthetically pleasing position.
In order to increase the size of the breast a number of techniques are available:
Implant
Fat transfer or ‘lipofilling’
Combination of implant and lipofilling (composite breast augmentation)
Microsurgical tissue transfer
External expansion
The Surgical Technique
Implant based breast augmentation
Breast implants are like small balloons. The outer layer is soft and elastic but very strong. Different styles of implants have outer layers which differ in terms of their thickness, texture and flexibility. Some have an additional outer coating of titanium or polyurethane foam.
The prosthesis is filled with either saline (salt-water) or silicone gel. In the past, liquid silicone gels caused problems when the outer shell ruptured. These days the gel is cohesive so that even if there was no outer shell, the gel would stay together. It is soft and malleable, but not fluid.
The shapes and volumes of implants vary greatly. Some are round while others have a tear-drop profile. There are numerous manufacturers and surgeons may have their preferences but will discuss these options with their patient. Although many varieties are available, in our opinion, an implant that is too big will lead to a less natural result and very large implants can lead to increased complications.
The surgical technique is straightforward. Through a small incision, a pocket is made behind the breast and the prosthesis inserted. The most common sites for the incision are (fig. 1):
Near the armpit
In the crease under the breast
Around the areola
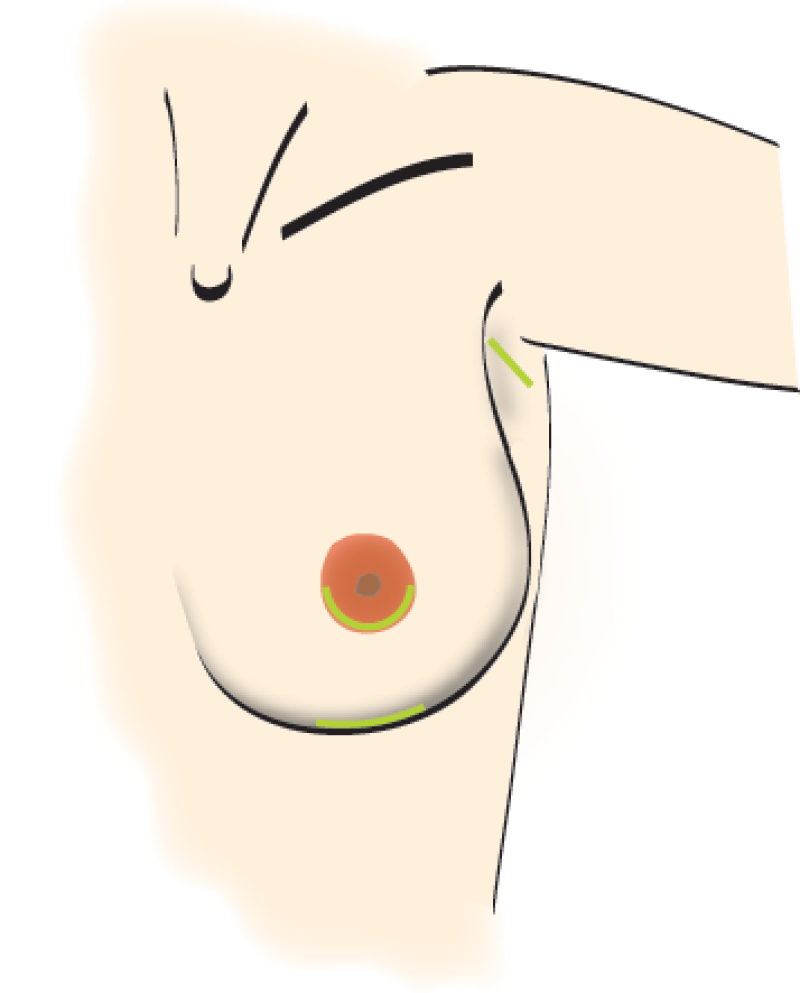
Fig. 1
Implants can be placed via the navel, but this is technically difficult and the results are therefore often not as good. This and the armpit incision are only really suitable for saline-filled implants. If they later need to be corrected, the subsequent incision would have to be in the breast crease or nipple. Areola incisions settle well, but sometimes affect the sensation to the nipple. It is for these reasons that the incision in the crease under the breast is our preference.
The implant may be placed either over (fig. 2) or underlying (fig. 3) the pectoral muscle. If there is enough breast tissue and good quality skin, the implant is best placed underneath the gland. If the overlying tissue is thin, the implant is better placed underneath the muscle. Sometimes a combination of these two locations is the best way to achieve a good result. The position of the prosthesis has little bearing on the risk of complications.
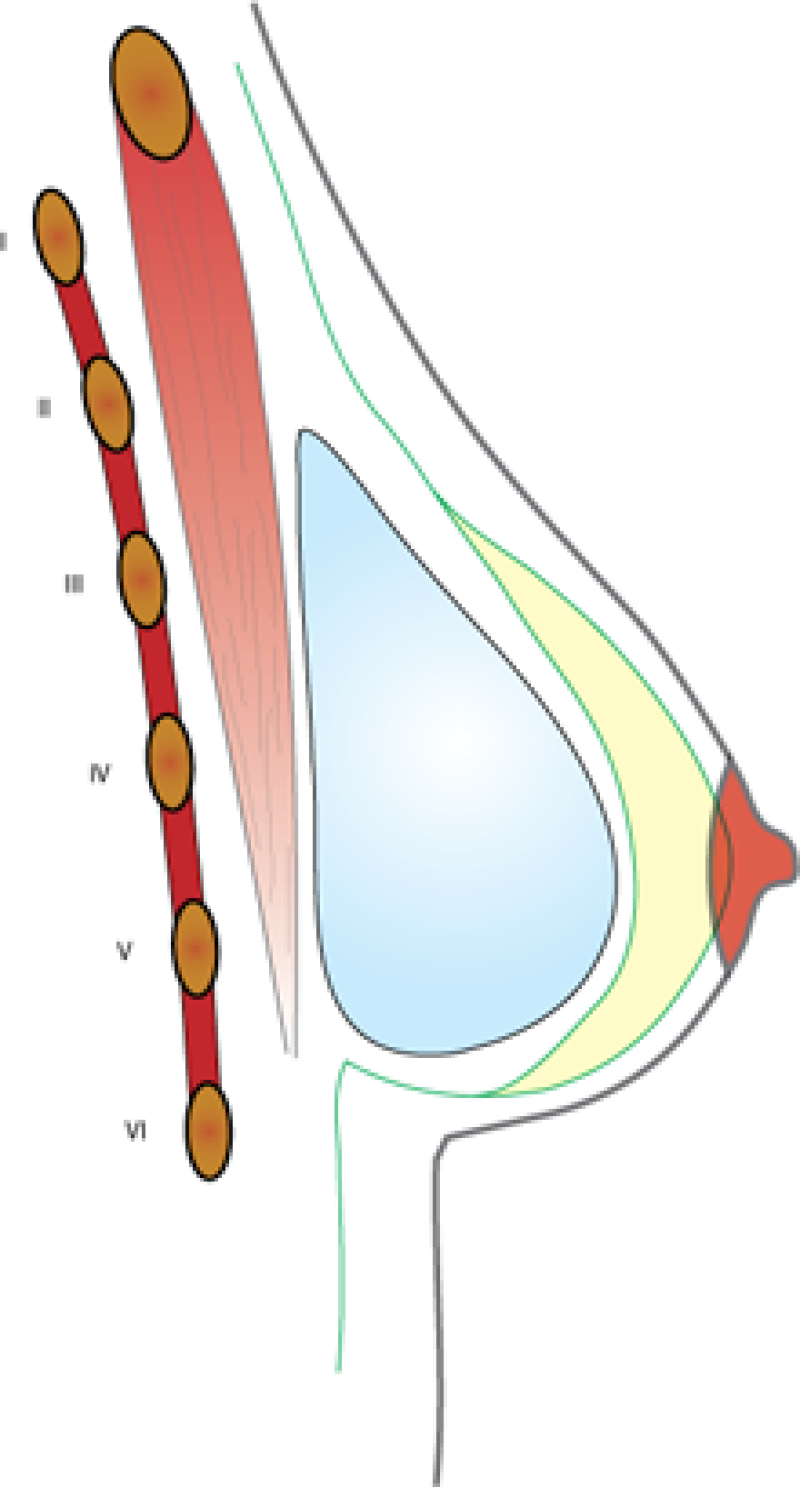
Fig. 2: Position in front of pectoral muscle
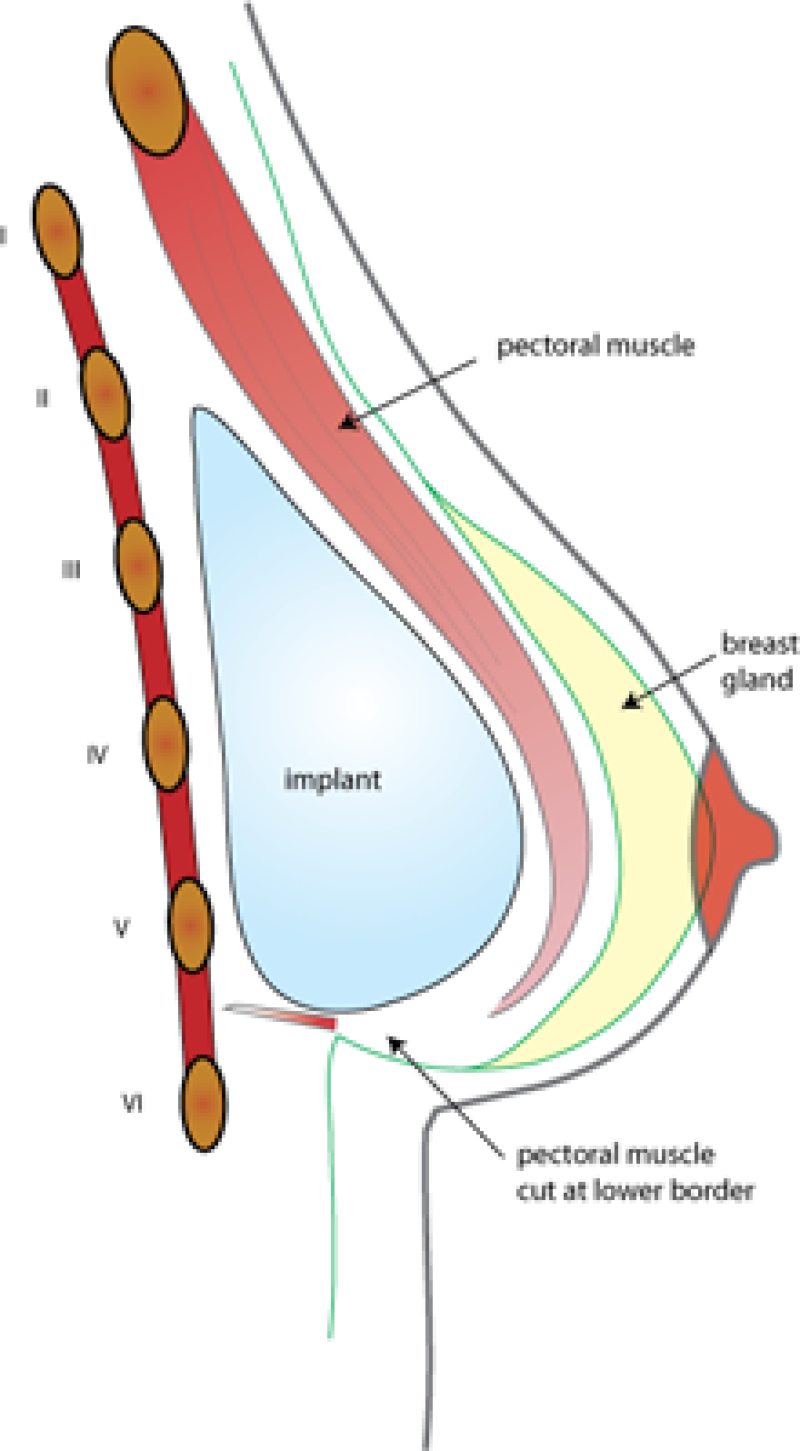
Fig. 3: Position behind the muscle
Finally, sometimes a surgeon will decide to leave a small drainage tube coming out through the skin to avoid any collection around the breast implant. This will be removed after one or two days.
Augmentation through lipofilling
With this technique, fat cells are removed from another part of the body, processed to isolate them from their surrounding liquids and injected into the breast just underneath the skin. The main advantage is that no foreign material has to be inserted and that rejection cannot occur. However, not all of the cells survive the procedure and only around 40-60% will remain. Once it has survived after 6 months, it will last a lifetime. The drawback is that only a limited amount can be injected on each occasion. Around 100-150cc is the maximum. Only very small scars are left where the fat is harvested and where it is injected. Although the technique is not very complex, it is very time-consuming.
The ideal patient for this procedure is a young woman with excess fat around the abdomen or hips who has small breasts and only desires a modest increase in their size.
More information can be found on www.lipofilling.com
Composite Breast Augmentation
The prosthetic breast implant may be the single most important device ever developed in the field of plastic and reconstructive surgery. Despite half a century’s worth of technological advances, the revision rate for breast prostheses remains high: 24% at 4 years and 36% at 10 years. Many revisions are performed for soft tissue related problems and not for failure related to the device per se. Soft tissue problems include capsular contracture and chronically atrophied and inadequate overlying tissue sometimes causing visibility of the device, a condition we define as "soft tissue failure". Simply stated, one of the major drawbacks of breast implants is their unnatural appearance when the overlying soft tissue volume to implant volume ratio is out of balance.
Early work with lipofilling focused on core volume enhancement but there is a natural limitation to the projection achieved with fat alone, due to its soft nature. Making the analogy to “mountains of sand”, breast projection using only fat comes at the cost of a wide breast footprint, often wider than desired.
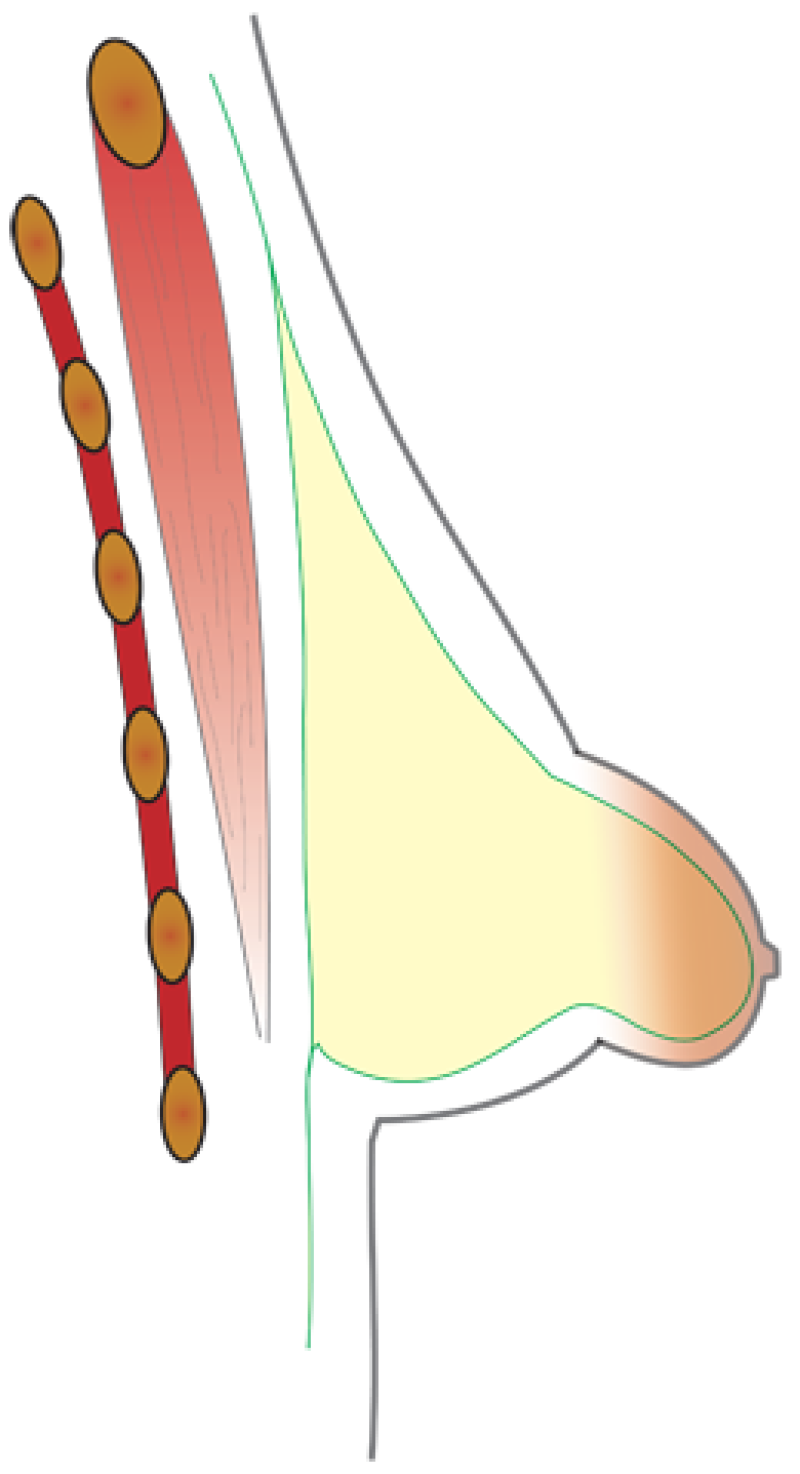
Over the last 5 years we have successfully been using a combination of classic implant and simultaneous management of the overlying soft tissue with lipofilling - a concept we define as composite breast surgery. By incorporating both mediums, one may achieve the core volume projection of an implant complemented by the natural look and feel of a fat overlay.
The technique is simple: the implant is placed in a pre-muscular plane, avoiding post-operative movement of the implant with movements of the arm. Also, this positioning is much less painful. Lipofilling is mainly added on the superior border of the implant to increase the soft tissue coverage of the implant. Fat can also be added in the other quadrants of the breast to improve the implant versus soft tissue ratio. Smaller implants with thicker soft tissue coverage will be less prone to long term complications.
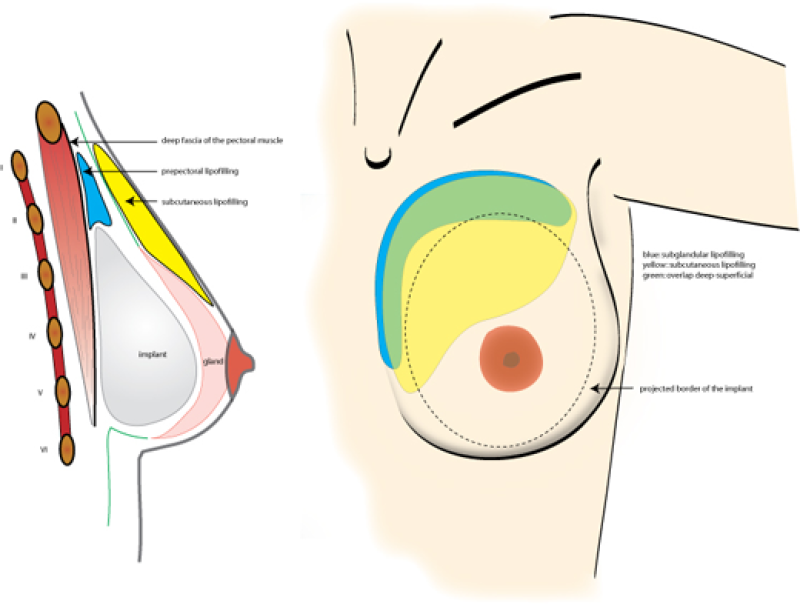
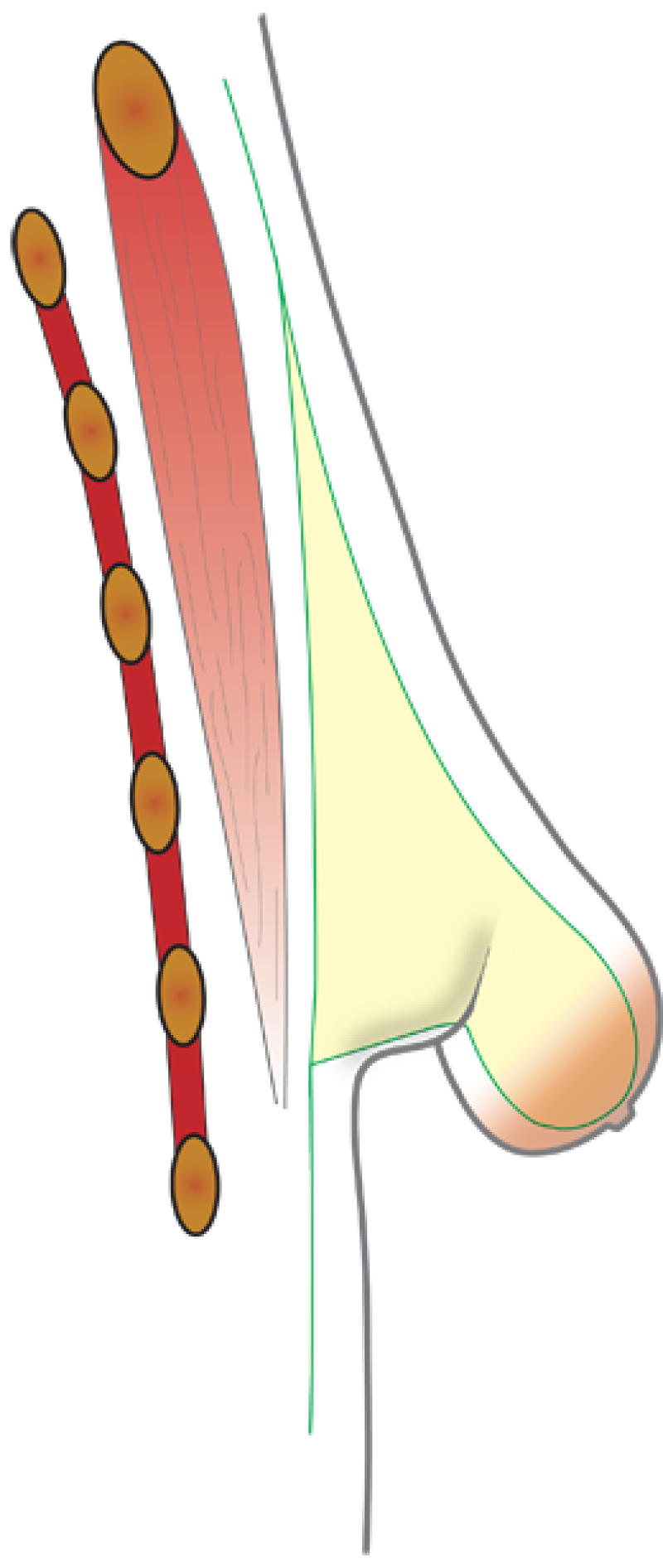
Figure 4. Frontal and lateral views of implant insertion in composite breast augmentation. Deep lipofilling, just in front of the muscle (blue) and subcutaneous lipofilling (yellow) are mainly performed on the upper and medial border of the breast to cover the border of the implant and to provide a natural appearance of the décolleté area., |
Augmentation using microsurgical techniques
Our experience in the field of breast reconstruction allows us to use tissue from the buttock or abdomen to add volume to the breast.
A detailed explanation of these techniques is available in the reconstruction section. Briefly, a piece of skin and fat can be taken from the abdomen, the buttocks or the inside of the thigh, following detachment of its blood supply. This is then re-attached to another vessel adjacent to the breast, so that the transplanted tissue survives on its new blood supply.
The main disadvantage is that this is a long, complex procedure and leaves a major scar at the donor site. However, it has the advantage of providing enough tissue in one operation to increase the size of both breasts by between 300 and 800cc. The tissue is your own and no immune rejection will occur and again the tissue will last a lifetime.
The ideal patient for this approach would be a lady who would deem the tummy-tuck that is performed at the donor site as an advantage. This is particularly the case after multiple pregnancies, weight loss or as one enters middle age.
Augmentation by external expansion
This went through a phase of being popular some years ago. An external expander applied suction to the outside of the breast to achieve an increase in size. However, the results proved to be unpredictable and short lived and therefore the technique is now rarely performed.
Breast augmentation in combination with a mastopexy
The details of a breast lift have previously been covered. It allows the position of the nipple to be moved and the implant is inserted through the vertical scar of the mastopexy.
Combining an augmentation and a mastopexy is the ideal solution for the sagging, small breast, however it is not as simple as it appears.
It is a much more technically demanding procedure than either component on its own. It can be difficult to achieve a pleasing shape and symmetry. There is also the trade-off of additional scarring along vertical lines and around the nipple.
Examples

Fig 5a

Fig. 5b

Fig. 5c

Fig. 5d
Figures 5: Pre (a) and postoperative (b, c, d) images of a breast augmentation with a 280 cc anatomically shaped cohesive gel silicone implant placed beneath the pectoralis major. |

Fig. 6a

Fig. 6b

Fig. 6c

Fig. 6d
Figure 6: Pre(a) and postoperative (b, c, d) images of a breast augmentation using a pre-pectoral implant. |


Figure 7: case 1: Pre(above) and postoperative (below) images of a composite breast augmentation, combining breast implants and lipofilling. |


Figure 8: case 2: Pre(above) and postoperative (below) images of a composite breast augmentation, combining breast implants and lipofilling. |


Figure 9: Pre(above) and postoperative (below) images of an augmentation mastopexy, combining breast implants with a breast lift procedure. |


Figure 10: Pre(above) and postoperative (below) images of another case of augmentation-mastopexy, combining breast implants with a breast lift procedure. |
What to expect after the surgery
There is usually a dressing applied over the scars. Drains may also have been placed - tubes which come out through the skin to remove any excess fluid. A band, or tape around the breast will hold the implant in place. After these are removed a well-fitting sports bra should be used.
Normal sequelae of the surgery include bruising and swelling. There may be sensory changes to the skin of the chest or the nipple. These are usually temporary. Minor aches and pains after any surgery are to be expected and can be treated with pain killers. If the implant has been placed under the muscle you may be discouraged from moving your arm in certain directions for the first few postoperative days.
Length of Stay
For implants alone or lipofilling you would normally go home the same or the next day. Following a microsurgical procedure you would expect to remain in hospital for three to five days.
After discharge
If the wound has been covered with paper tape, this can be removed by washing after 1 week. Depending on the type of skin closure, you may be given additional advice by your surgeon.
As mentioned earlier, you will need to wear the right support which can be provided by a sports bra. A normal underwired bra can be worn after the first two months. Strenuous exercise and sport should be avoided for at least two weeks and it is better not to sleep on your stomach for the first 8 weeks.
One to four weeks should be taken off work, but daily household tasks can be resumed within the first few days.
Sensory changes experienced immediately after the operation will wear off over time. This will take longer if a larger implant has been used and can rarely be permanent.
Breastfeeding is not affected by breast implants.
Possible complications
Early
Bleeding
Infection
Wound healing problems
Skin irritation
Late
Persistent sensory disturbance
Asymmetry
Dissatisfaction with volume
Scar hypertrophy (thickening)
Persistent pains
Capsular contraction
Implant movement, rupture, leak or becoming more palpable
There is no proven link between breast implants and any systemic diseases. There have been numerous scares in the press, but none have been unequivocally linked.
Final Points
This is a purely cosmetic procedure which your healthcare insurer will not fund. Both the medical costs and fees must be met by the patient. Costs vary from case to case and an agreement will need to be made in advance with your surgeon.
Read more (links)
Read more on the Safety of Silicone Gel-Filled Breast Implants
Read more on breast implant complications
Read more on questions to ask your doctor
Read more about things to consider before getting breast implants
C. Breast Reduction
Description of the Problem
Surgical planning depends on the type of breast hypertrophy (overgrowth)
Type 1:
The increase in volume is predominantly in the central and upper chest. Gravity draws the tissue downwards and the distance from nipple to collarbone increases greatly while that to the crease under the breast only increases slightly.
Type 2:
The gland has overdeveloped in the lower part of the breast. More skin stretch occurs below the nipple so the distance from the nipple to the fold increases.
Type 3:
A combination of the above, where both measurements increase significantly.
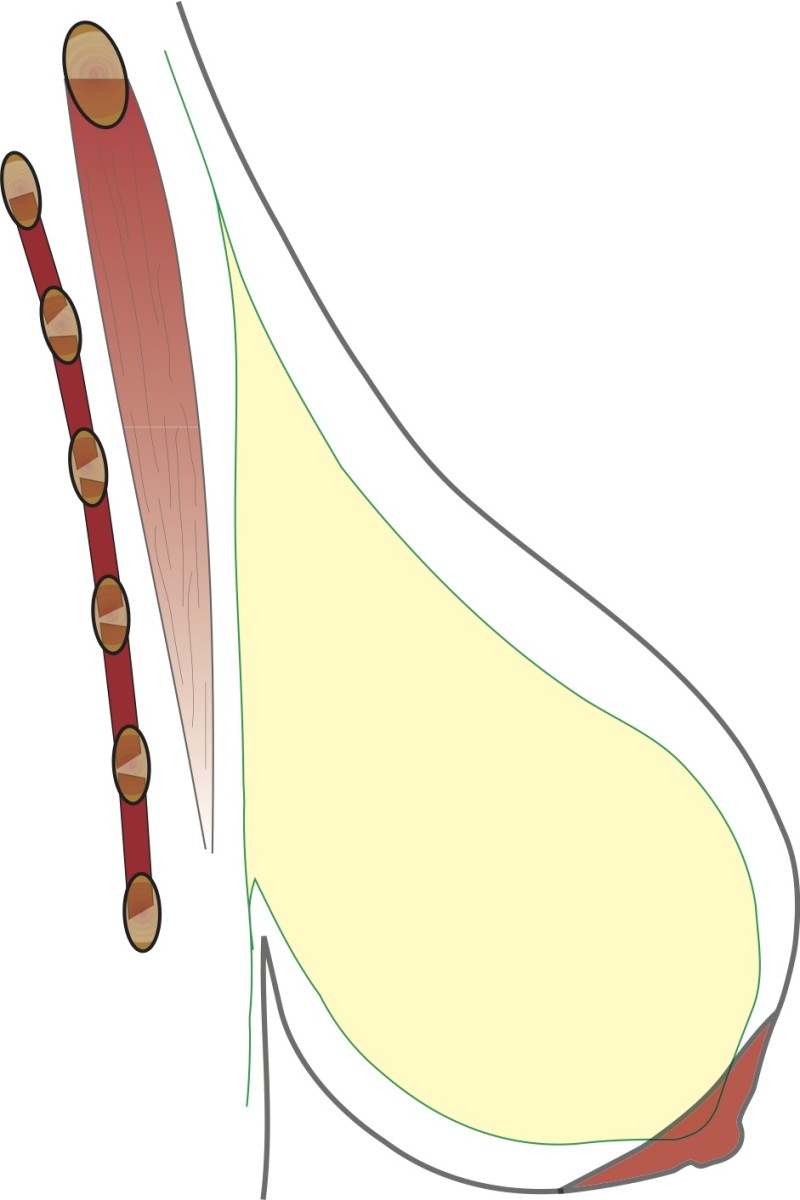
Fig. 1: Type I
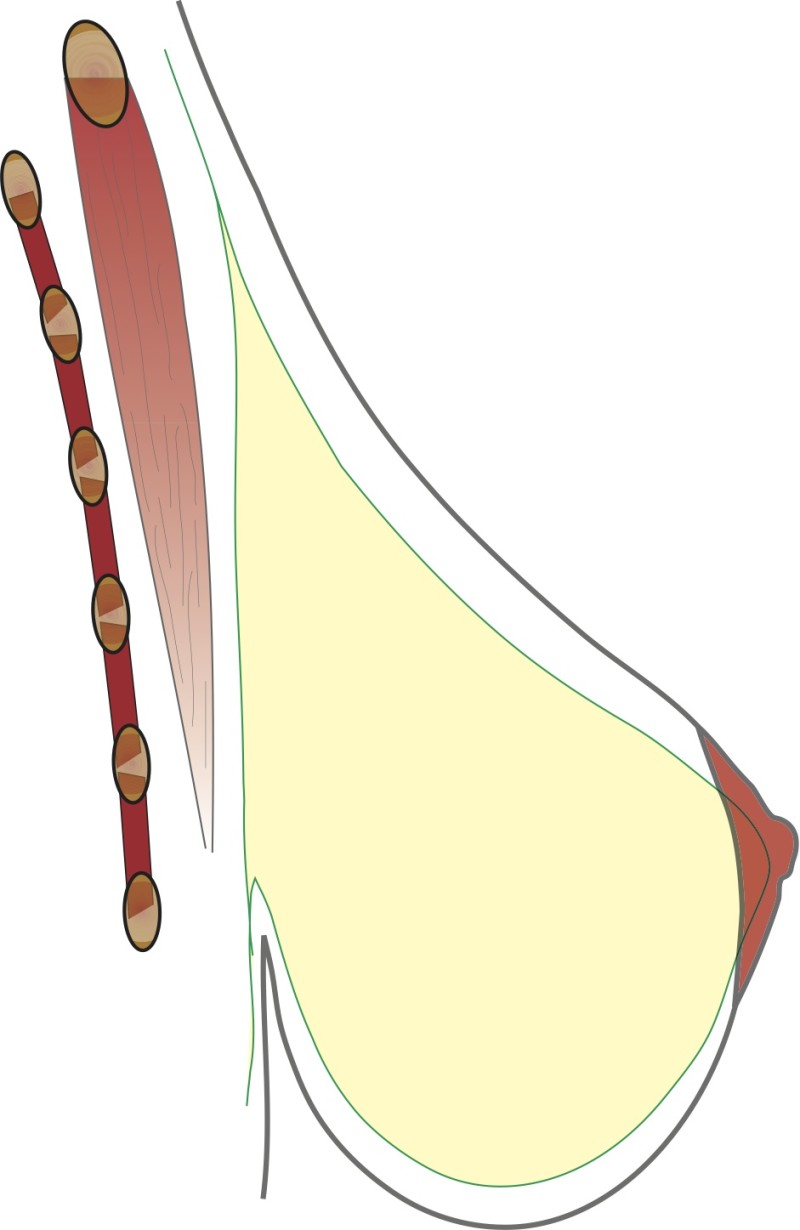
Fig. 2: Type II

Fig. 3: Type III
Figures 1,2,3: The three different types of breast hypertrophy |
Aims of Surgery
The problem results from an excess of both skin and tissue. Surgery therefore reduces the volume and in addition re-drapes the skin to produce a pleasing shape. In doing so, the nipple is repositioned and the areola reduced in size where necessary.
Technical Aspects of the Surgery
There have been considerable advances in the surgical techniques for breast reduction over the last 50 years. Initially, volume reduction was the principal aim. This was refined to also provide a pleasing shape. More recent advances enable us to achieve the above while minimizing the extent of the scarring. Focus is also maintained on maintaining the blood flow and sensation to the nipple and areola complex.
Before the operation the surgeon draws a number of complex planning marks on the patient’s chest. It is important to carry this out while the patient is upright as the relationships change when lying down for surgery. The measurements calculate the amount of tissue to be removed and the new nipple height. It is difficult to plan for a specific desired breast shape, but following consultation an approximate breast size can be agreed. Usually, a C cup is seen as the best balance between breast and chest size, but this can be modified to suit the patient’s preference.
The procedure has three principal components. A tissue ‘pedicle’ is designed to retain blood flow and feeling to the nipple. Excess skin and tissue are then removed, before the breast is finally brought into a pleasing shape and closed. A number of alternatives exist for each of these stages.
The blood supply to the nipple can be achieved through ‘pedicles’ arising from different directions and they can be designed in different thicknesses.
Likewise, breast tissue can be removed mainly from the top, bottom, or outside of the breast. After a wedge of tissue is removed, bringing the remaining tissue together produces a pleasant breast ‘cone’.
The excess skin can be removed in any of the ways described for a breast lift. There will be a scar around the areola and one extending vertically downwards. In some techniques called ‘vertical scar’ these are the only scars. Commonly though, an additional scar across the fold under the breast is needed to achieve the ideal shape. Overall, there are two techniques that are most commonly employed.
The vertical scar technique (of Lassus and Lejour)
Here the nipple and areola are left with a blood supply from above. A wedge of tissue is removed from the lower part of the breast and the only scarring is around the areola and vertically down to the fold under the breast. The main advantage is minimal scarring. The disadvantages are that blood flow to the nipple may be reduced as might sensation. Skin is only pulled in horizontally in the lower part of the breast so excess skin along the vertical line might allow sag of the overlying tissue to re-occur. The patients for this procedure have to be carefully selected.
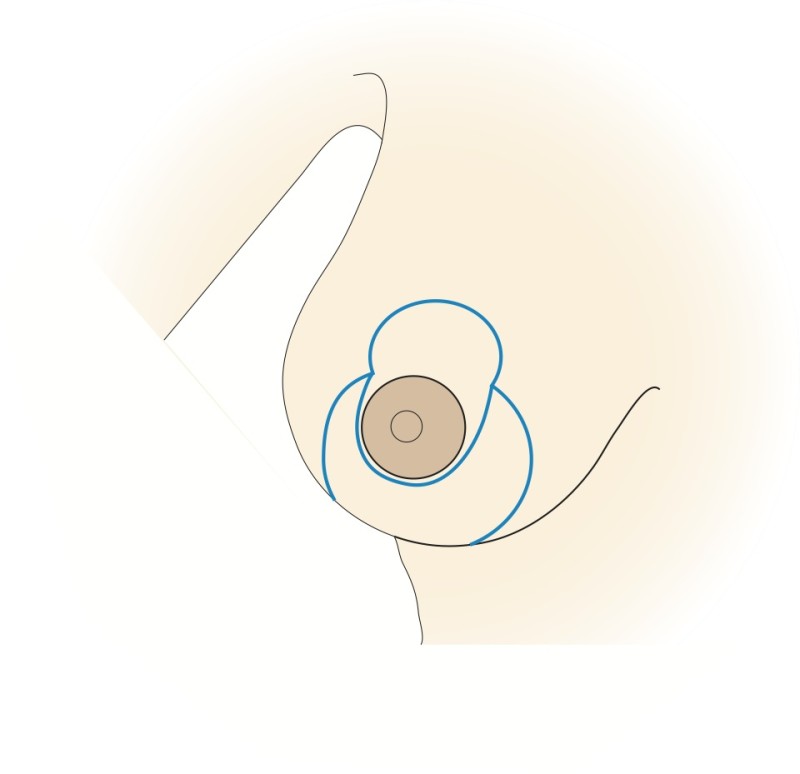
Fig. 4a
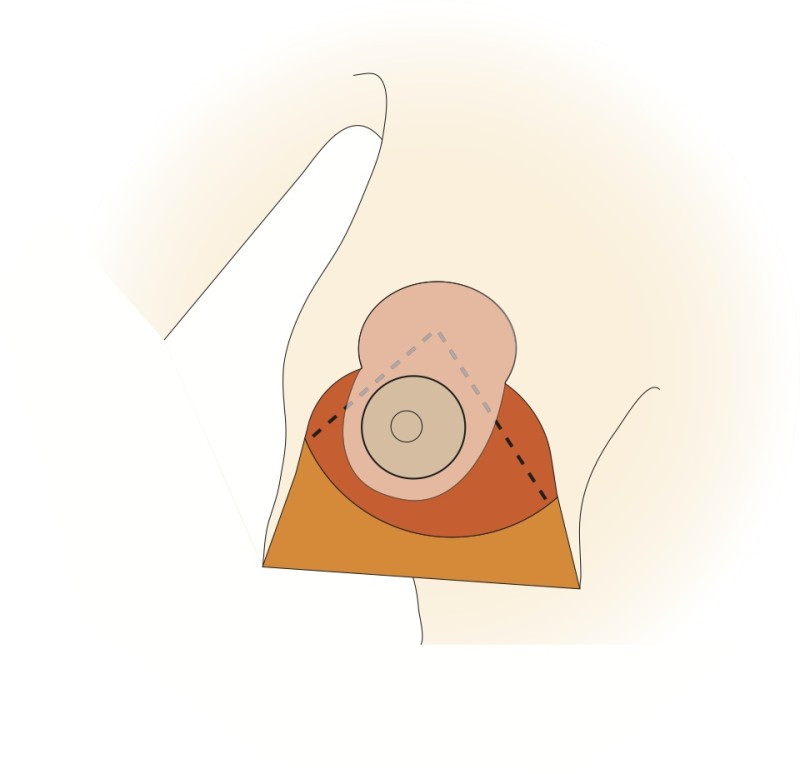
Fig. 4b
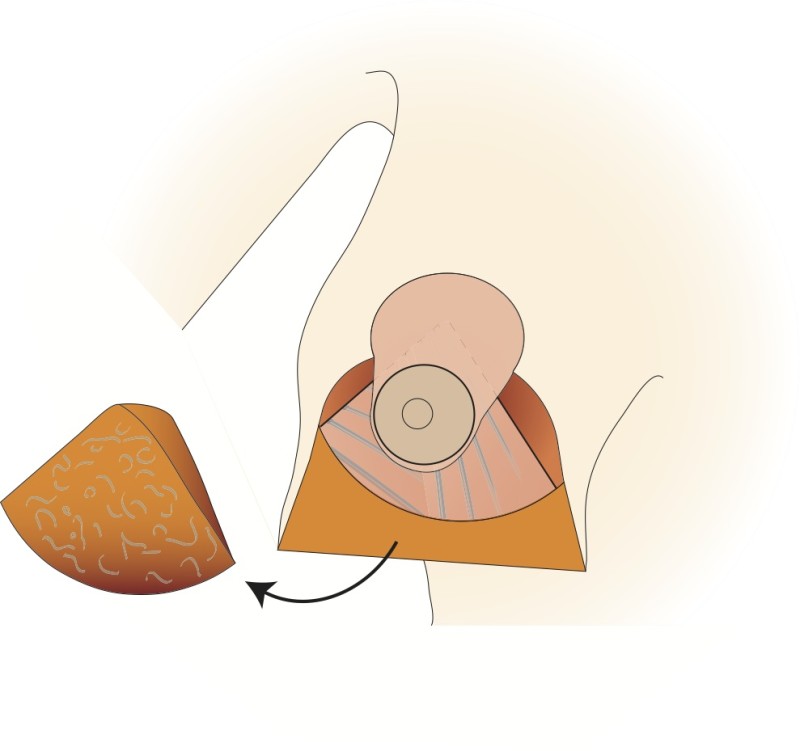
Fig. 4c
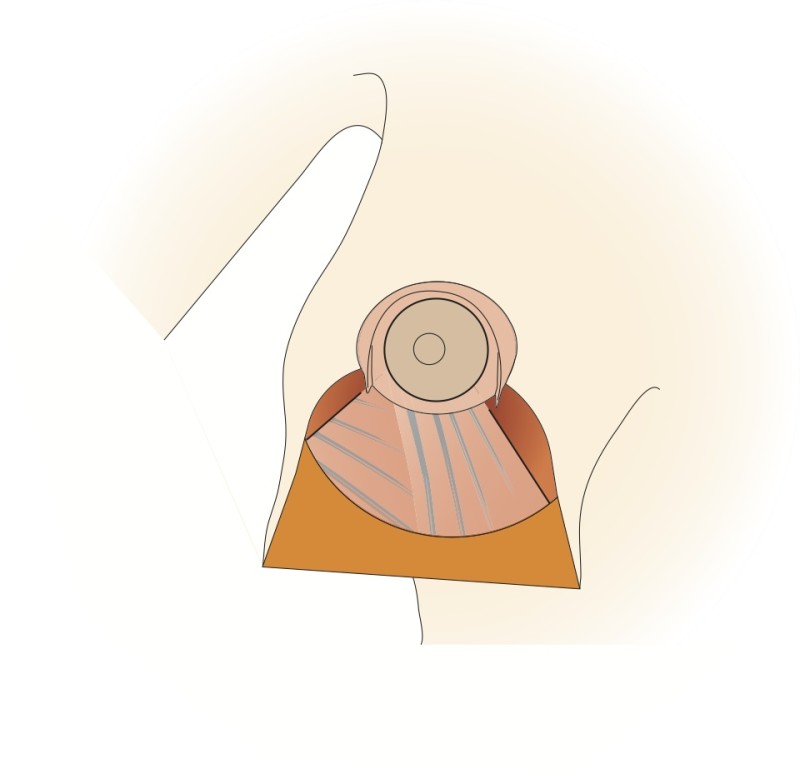
Fig. 4d
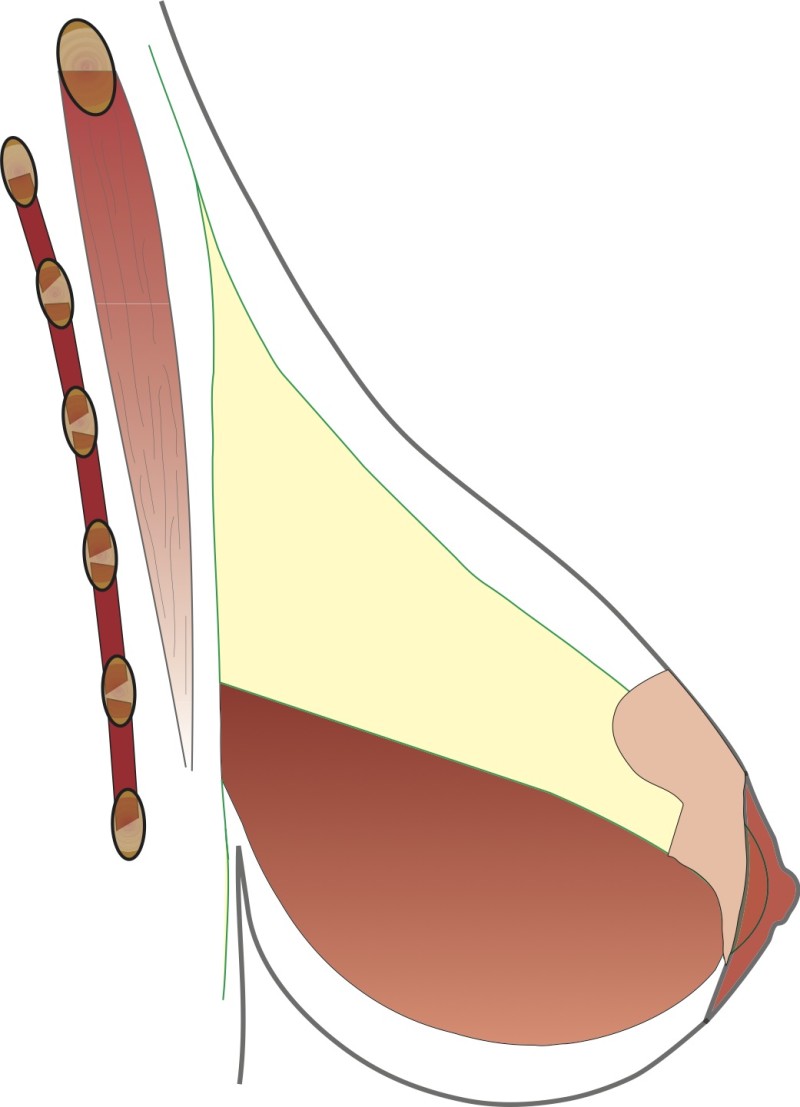
Fig. 4e
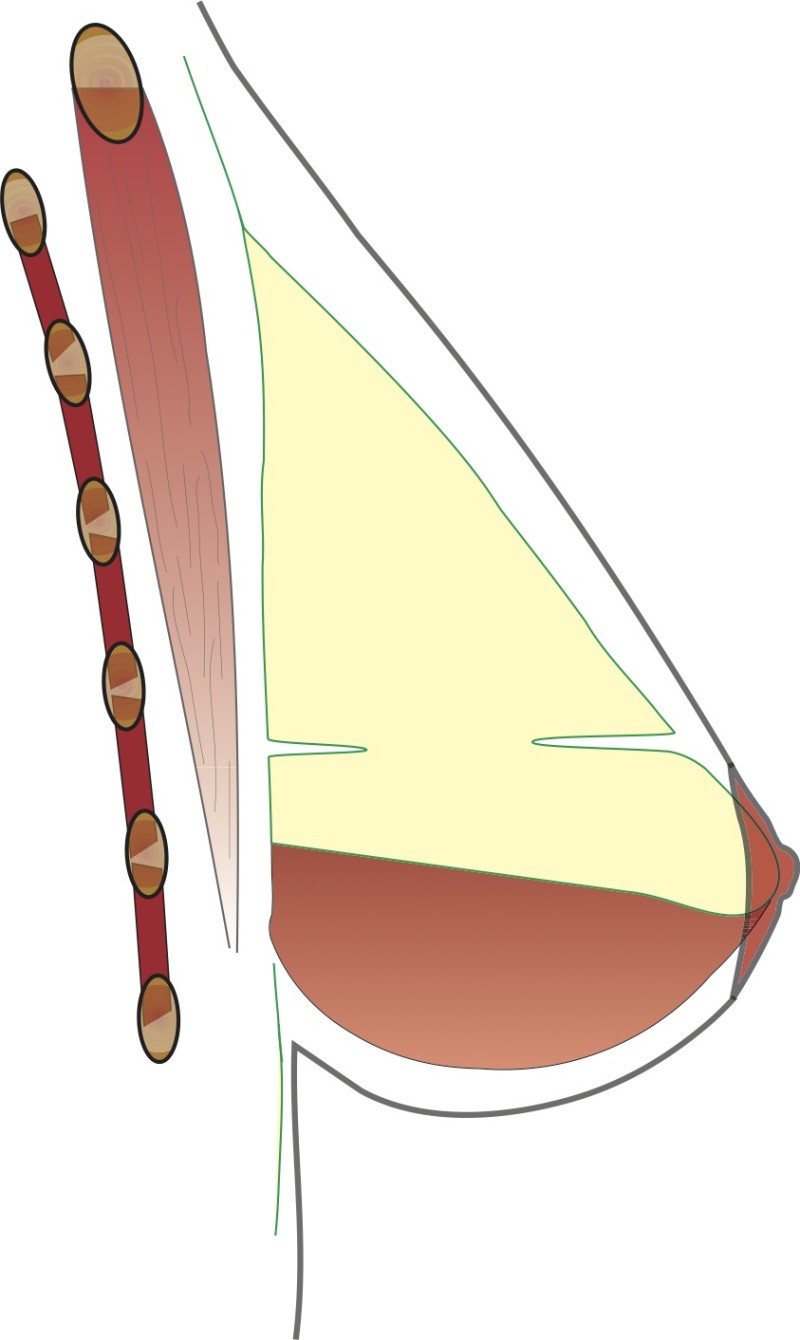
Fig. 4f
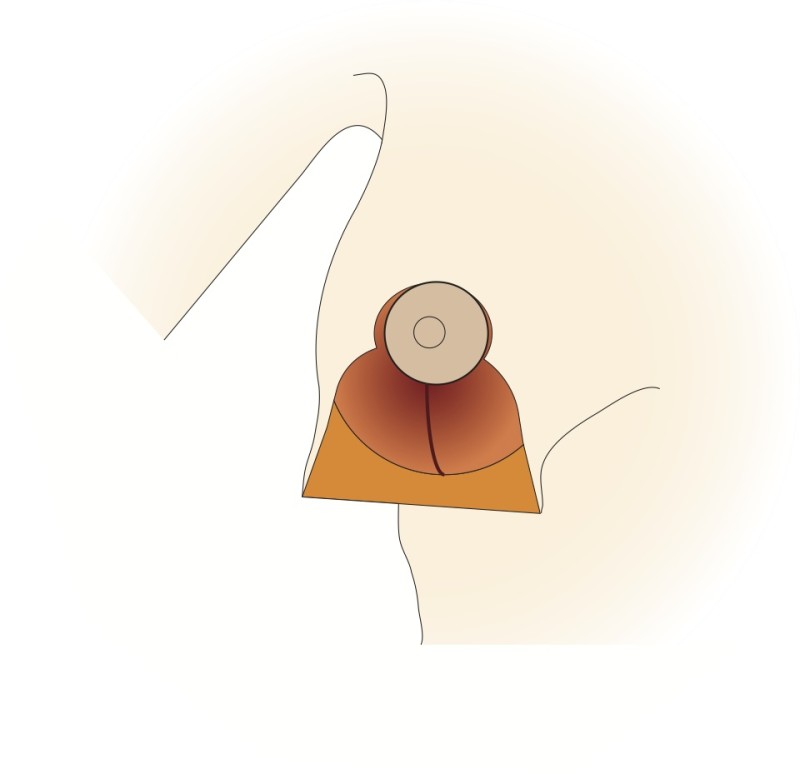
Fig. 4g
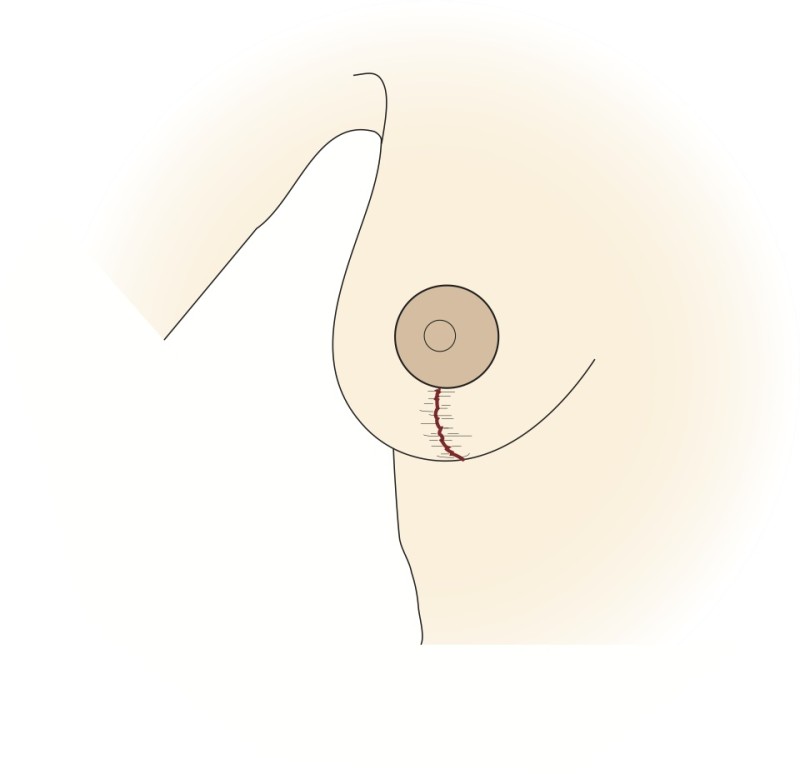
Fig. 4h
Figure 4: The vertical scar technique: (a) preoperative markings (b) the nipple is cut around and the skin underneath undermined; a pedicle of skin and a thin layer of intact gland are preserved (c, d) a wedge of tissue underneath the nipple is then removed; (e, f) the nipple is moved upwards by folding this tissue on itself; (g) The remaining tissue is brought together; (h) the skin is stitched with the wound deliberately ‘crumpled’ to shorten the final scar. |
Perforator based technique (of Blondeel)
Here the nipple and areola remain supported by ‘perforating’ vessels which come through the pectoralis major muscle from below. This technique also takes into consideration the sensory nerves to the nipple which can be preserved in most cases. Tissue is mainly removed from underneath and above the nipple. To optimally reduce the skin in the lower half, a scar of variable length in the crease underneath the breast is necessary. The main advantages of this modification lie in the robust blood and nerve supplies to the nipple and a natural shape to the breast and areola following surgery.
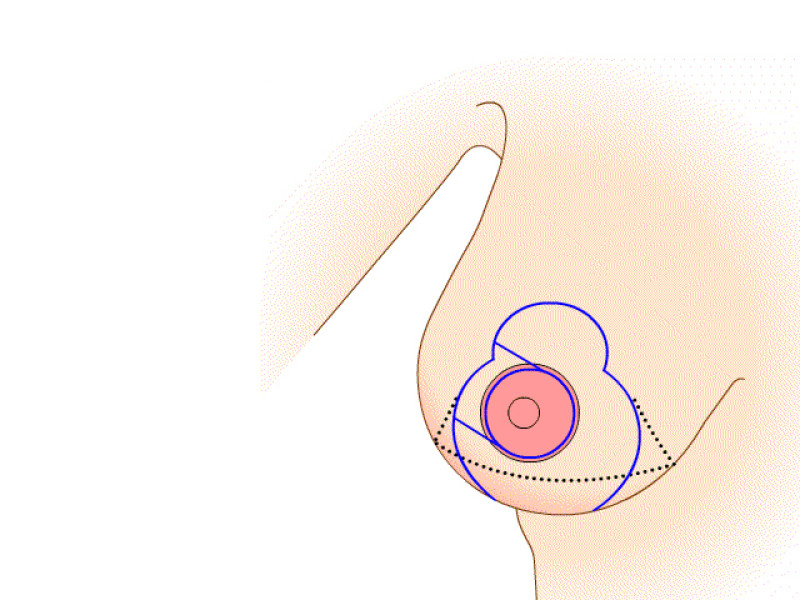
Fig. 5a
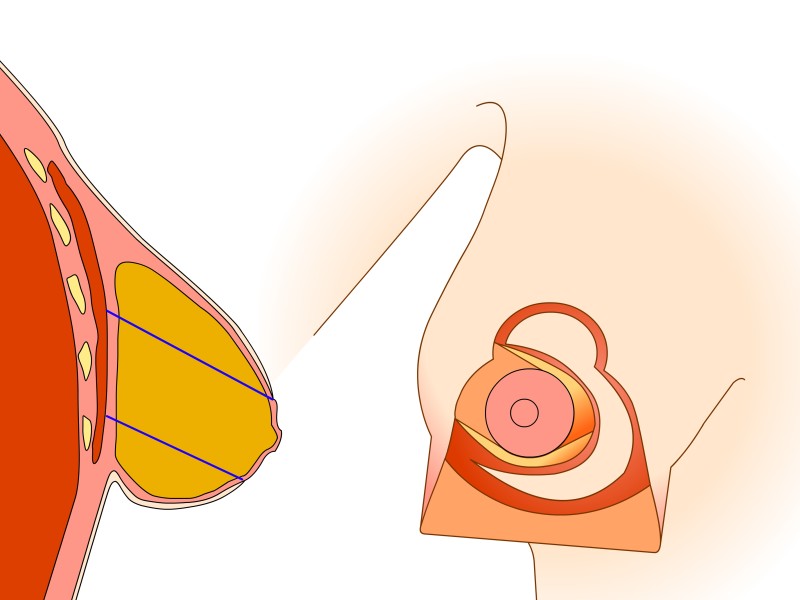
Fig. 5b
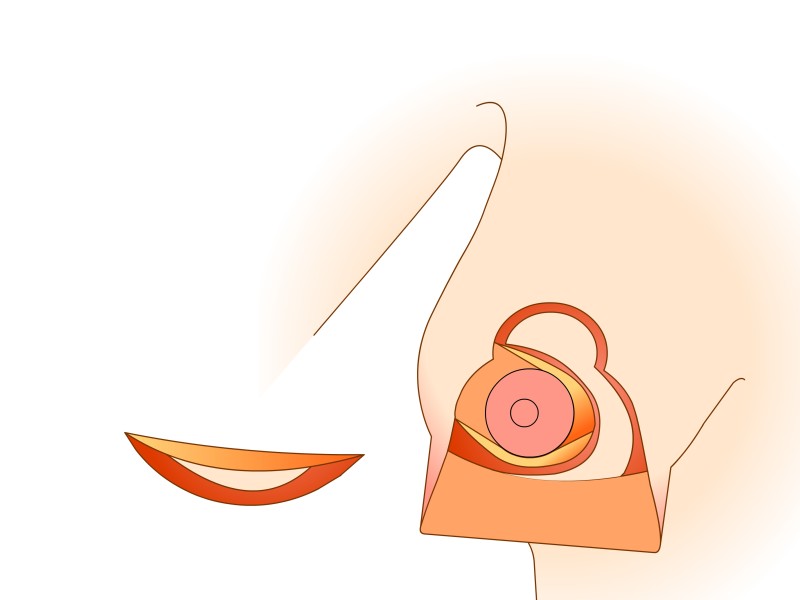
Fig. 5c
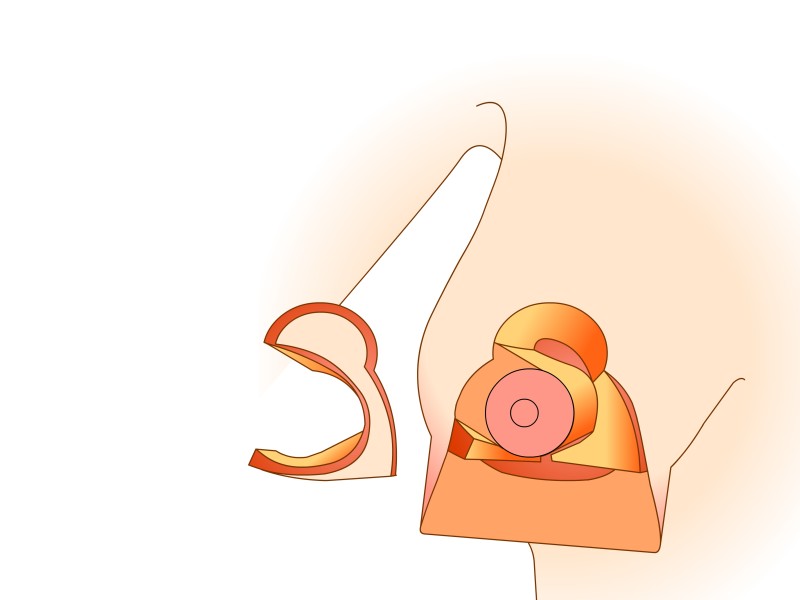
Fig. 5d
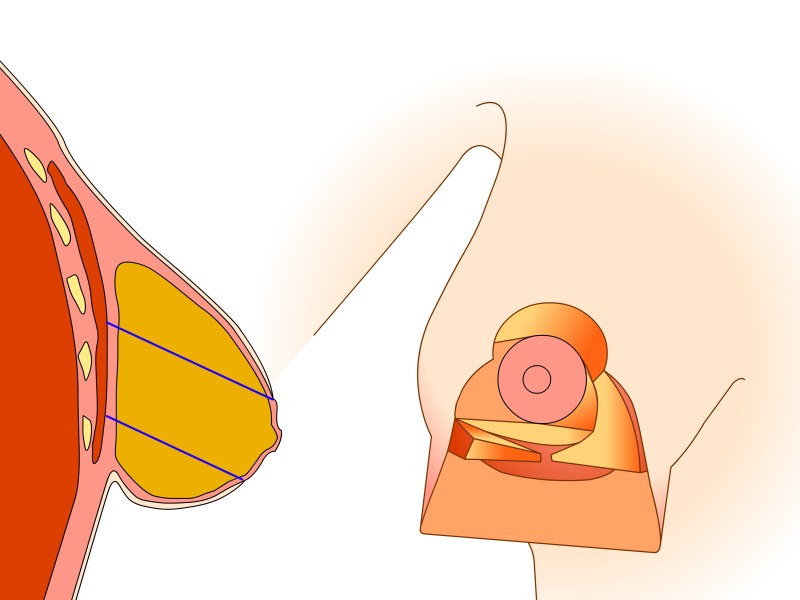
Fig. 5e
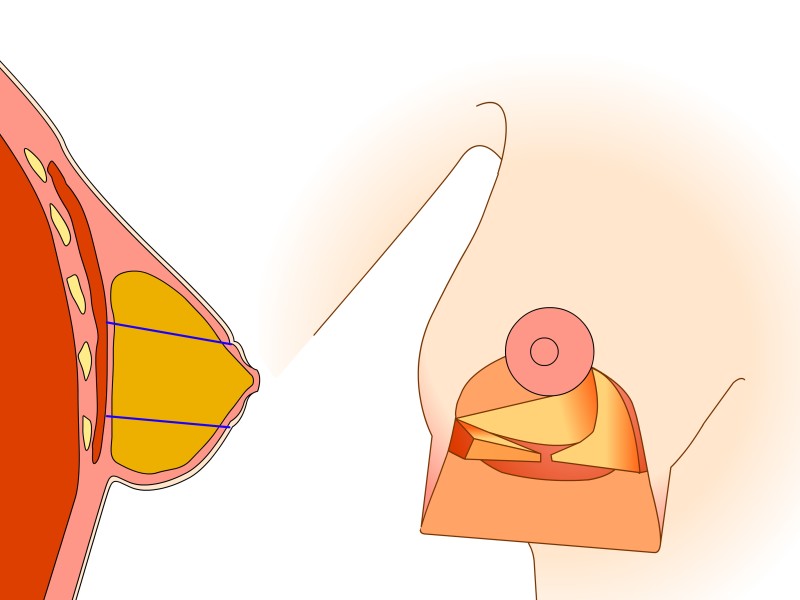
Fig. 5f
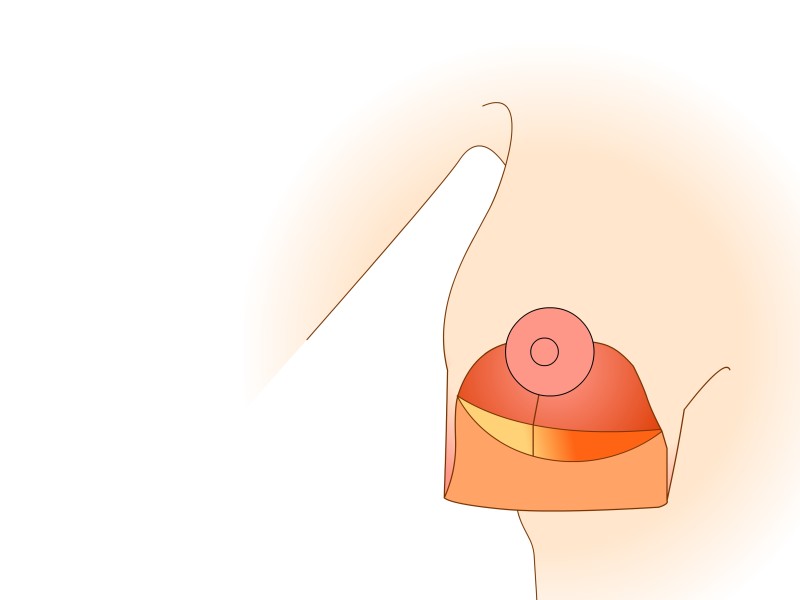
Fig. 5g
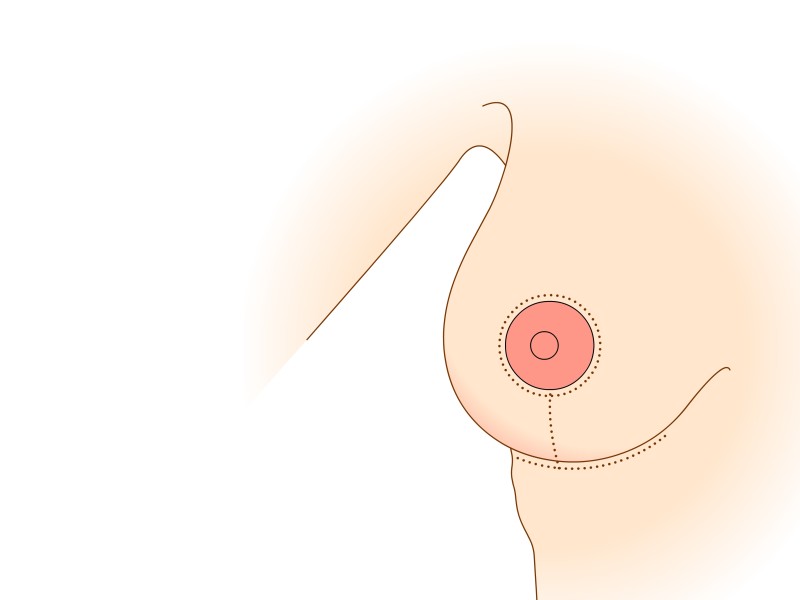
Fig. 5h
Figure 5: (a) Preoperative markings. (b) Skin is undermined and removed with preservation of the blood supply to the nipple (c) the lower, horizontal part of the gland is removed (d) vertical part is removed taking away breast gland below, medial and above the nipple-areola complex (e, f) the column of tissue with the nipple still attached is tilted upwards (g) the remaining tissue is brought together (h) the skin is closed with an ‘anchor’ shaped or inverted-T scar. |
What to expect after surgery
There will be a dressing along the wounds on each breast. Some elastic tape or a special bra may be used to support the breast. There will often be tubes coming out through the adjacent skin to drain off any excess fluid that accumulates following surgery. These can be removed between 24 and 48 hours afterwards.
It is normal to see the following after surgery:
Bruising, mostly around the areola, but the colour can spread across the chest. Swelling of the breast also commonly occurs. This gets worse over the first few days then gradually improves.
Temporary loss of sensation of the nipple, areola or surrounding skin. This is common and can take weeks to months to fully recover, depending on the procedure. There will also be some pain after the operation. The initial ache fades, but as the scars mature there will be occasional stinging pain over the following months.
Examples


Figure 6: Pre(above) and postoperative (below) pictures of a prominent Type III breast hypertrophy who underwent a breast reduction using the Blondeel technique. |


Figure 7: Pre(above) and 11 years postoperative (below) pictures of a Type I breast hypertrophy who underwent a breast reduction using the Blondeel technique. |
Length of Stay
The operation takes between 1.5 and 2.5 hours and the length of hospital stay is between 24 and 48 hours. The amount of fluid coming out through the drains usually determines this length of stay. Once it has slowed to an acceptable amount, they can be removed and the patient can go home.
Aftercare
If the wounds have been covered with protective glue, the top dressings can be removed to shower the following day. In other cases the wounds may need to be kept dry for a longer period.
Elastic tape can be replaced by a supportive (sports) bra when leaving the hospital. Surgeons vary in their preferences regarding the support of the breast and each will advise you accordingly. Usually, you will be asked to wear a bra day and night for up to 4 weeks. Normal bras can be worn again after 3 months.
For the first 48 hours, physical activity, particularly arm movements should be limited to a minimum, but after this, full mobility is encouraged. However, no heavy work or sports should be done for 3 weeks postoperatively. It is also not recommended to sleep on your stomach during the first 4 weeks. Depending on your type of work, 2-3 weeks should be taken off to fully recover.
Potential Complications
Early:
Local
Bleeding
Infection
Wound healing problems
Skin irritation
Nipple/areola necrosis
Wound breakdown
General
·Deep vein thrombosis
·Lung embolism
·Chest infection
Late:
Nipple or skin numbness
Painful twinges
Other sensory disturbances
Scar hypertrophy (thickening)
Asymmetry
Dissatisfaction with the final volume
Subsequent changes in shape with gravity and ageing
Financial Considerations
Although breast hypertrophy is not a disease per se it frequently causes unpleasant symptoms and disability to the sufferer. As such, some health care systems including those in Belgium, Holland and the United Kingdom will fund the procedure after considering each case on its individual merits. In some instances, however, all or part of the cost will need to be met by the patient. Policies vary between insurance companies and you should check first with your provider. Be sure to have everything clearly documented in writing by both your surgeon and insurer.
One Patient’s Experience
I decided to have a breast reduction not only because of the pain in my shoulders and the inflammation underneath my breasts, but also to improve their appearance. My breasts grew rapidly from a young age and I had finished with an F cup and inverted nipples.
I had kept my breasts hidden since my adolescence. No one else knew how frustrated, embarrassed and unconfident I felt about my breasts. They seemed to define who I was, how I functioned emotionally, socially and in relationships. Thanks to the internet, I found a solution.My first meeting with a plastic surgeon was the hardest. I was so nervous that I struggled to hold back tears. Eventually, I regained control and was able to have an informed discussion about the operation.
At first I did not want anyone to know what I was doing, but then it became practically necessary and everyone was very understanding.I decided with my surgeon to aim for a C cup. Before the surgery careful markings were made on my breasts. I was nervous about the anaesthetic, but soon drifted off and awoke to the first glimpse of my breasts.
At first I was scared, they looked shapeless and bruised. The pain was quite tolerable which was a big relief ! It was literally a weight off my shoulders.
In my post-operative visits, my surgeon reassured me that everything had gone well. Over the next 6 months my breasts took shape and I am very proud of them. My scars are healing nicely. The only remaining problem was my inverted nipples. The surgeon suggested that nipple piercings would help this and that it was a minor procedure under local anaesthetic.
I cannot and will not hide the fact that I have had plastic surgery. My breasts have been corrected and I am so happy with the result. I feel more confident. If I had known earlier what I know now, I would have acted more quickly. I have never once regretted having surgery.
Read more...
D. Breast Lift
Description of the Problem
Breast lifts (mastopexy) correct a breast that is ptotic or sagging. There are three main types which determine the best surgical approach
Type 1:
The breast tissue and nipple both move downwards. The distance from the nipple to the collarbone increases.
Type 2:
The nipple stays in position while the breast tissue slides downwards underneath it. Here the distance between the nipple and the fold below the breast increases.
Type 3:
This is a combination of the above types
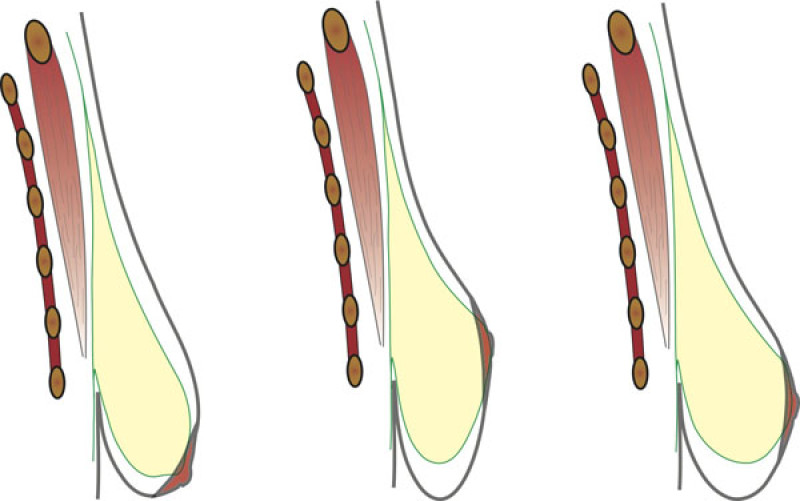
Figure 1: The three types of sagging breasts |
Aims of Surgery
A breast lift aims to move the skin and breast tissue upwards while restoring the nipple to the correct position, where necessary.
Surgical Technique
In lifting the skin of the bottom half of the breast, scars must be made both horizontally and vertically. The amount of droop or sag will dictate the length of the scars required. The more skin excess there is, the longer the scars necessary. The nipple and areola can also be re-positioned. Before the operation, the surgeon will mark the breast to plan exactly how much skin to remove and whether to move the nipple.
During surgery, these markings help the exact amount of skin excess to be removed and the gland is then modeled. If necessary, the nipple is moved upwards, but rarely does it have to be detached from any of the underlying tissue so that the feeling and blood supply are safely preserved. Once everything is correctly positioned, the skin is re-draped back and sutured. The surgical result is checked using a special tilting surgical table and any necessary refinements performed.
Depending on the nature of the breast sag, there are several different types of operation available:
Peri-areolar mastopexy
This only leaves a scar around the nipple and areola. It benefits from the minimal scarring. Main disadvantage of this technique is the flattening of the breast and nipple-areola complex and stretching over time of the areola into a wide, flat disk. It is only suitable for young patients with an elastic skin and with a very mild droop.
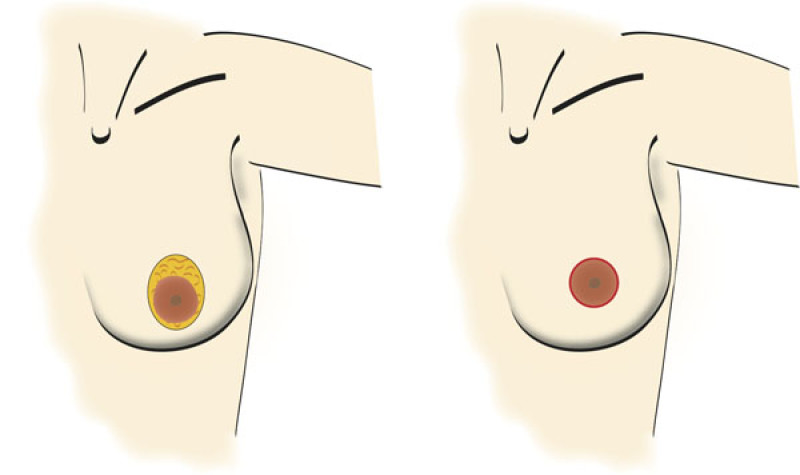
Figure 2: A peri-areolar mastopexy |
Vertical scar mastopexy
Here the scar runs around the areola and vertically downwards a variable distance towards the crease underneath the breast. This technique is well suited to Type I problems, but can be less useful in other situations.
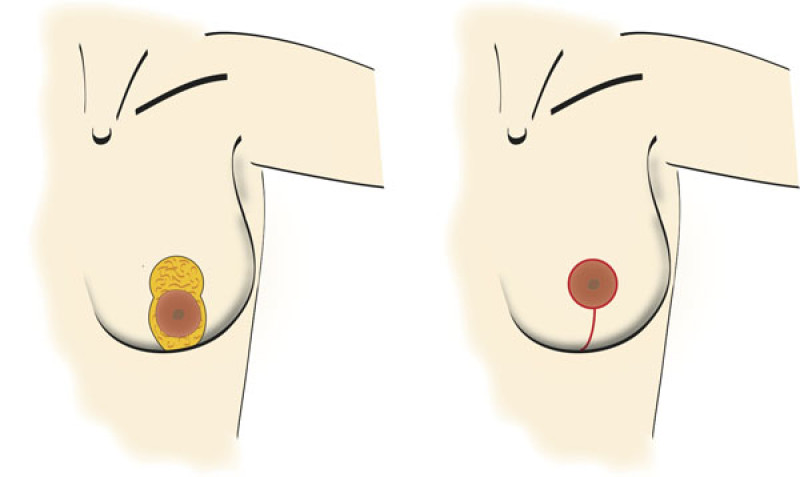
Figure 3: With a vertical scar mastopexy, excess skin is only removed in a horizontal direction. |
Mastopexy with an ‘anchor’-shaped scar
This adds a horizontal scar along the crease underneath the breast to the vertical and periareloar scars, creating an anchor shape.
This provides the greatest flexibility in reducing skin excess and is well-suited to the Type II, Type III deformity and more severe cases.Even though the scars are more extensive, this is necessary for some patients to achieve the best improvement in breast shape. All the scars are well hidden by a bra or bikini.
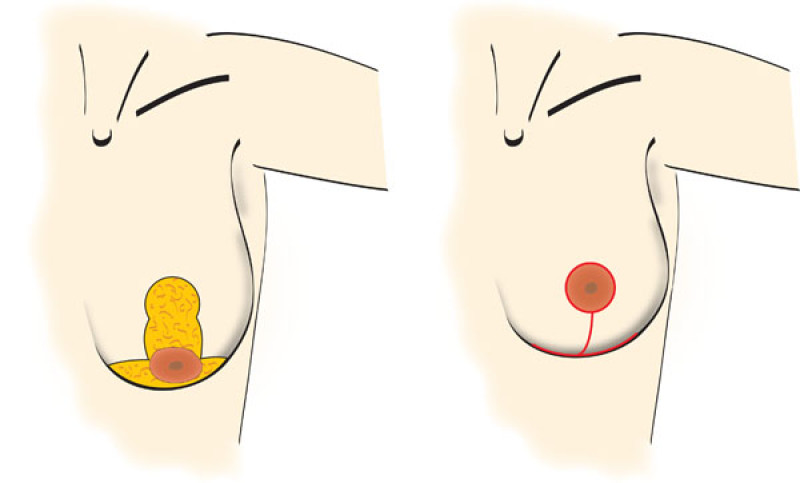
Figure 4: Mastopexy with an anchor-shaped scar: the excess skin is removed both horizontally and vertically. |
What to expect after Surgery
After surgery there will be dry dressings placed over the scars. If skin glue has been used to seal the wounds, the bandages can be removed to allow showering the following day. Otherwise, the wounds may need to be kept dry for longer. Depending on the extent of the surgery, you may need a drain through the skin, but this can usually be removed within 24 hours. There will be some supportive bands or tape over the breasts which can be replaced by a surgical or sports bra.
Normal things that can happen following surgery include:
Bruising, especially around the scars
A temporary loss of sensation
Swelling, which increases over the first couple of days, then gradually subsides
Mild pain will be experienced so analgesia is prescribed
Examples


Figure 5: case 1: Pre(above) and postoperative (below) pictures of a breast lift for Type III sagging breasts. |
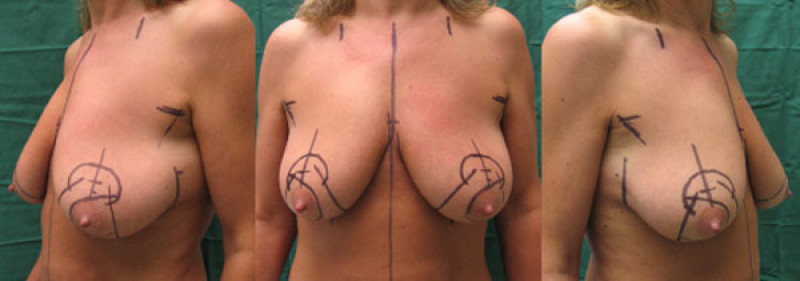

Figure 6: case 2: Pre(above) and postoperative (below) pictures of a breast lift for Type III sagging breasts. |
Length of Stay
Even quite extensive breast-lifting can be performed as a day case. This means that you can arrive in the morning and leave later in the afternoon. Rarely is it necessary to stay overnight.
After Care
As mentioned above, if the skin has been glued, you can shower the next day. Elastic tapes and bands can be replaced with a supportive sports or surgical bra. This should be worn both day and night for 3 weeks. After this time, you will be advised on how long to wear the supportive during the day before changing to a normal bra, usually this is around 3 months.
You will need to take between 2 and 10 days off work depending on your job. You should avoid strenuous activity and sleeping on your stomach for 3 weeks. The wounds should be completely healed in 2-3 weeks but this will determine the rate of your return to normal activities.
Potential Complications
Early:
Local
Bleeding
Infection
Wound healing problems
Skin irritation
General
Deep vein thrombosis
Lung embolism
Chest infection
Late:
Sensory loss (rare)
Ongoing pains
Abnormal sensations
Scar hypertrophy (thickening)
Asymmetry
Changes to the breast shape with aging
Financial Considerations
Breast ptosis or sagging is not a medical condition and does not cause any functional impairment. Therefore health services and insurers will not routinely fund this procedure. The entire operation including hospital stay, medical expenses and the fees must be covered by the patient. Since fees vary between surgeons and clinics, it is important to have a clear agreement in writing.
II. Congenital breast malformations
Developmental Malformation
The most common developmental breast deformations are:
A. Tuberous Breast Malformation
Description of the Problem
Tubular breast or tuberous breast is a more complex problem which has many variations. The lower part (one or both lower quadrants of the breast) of the breast does not fully form and appears constricted by tight overlying skin. The fold under the breast can be shifted upwards and the remaining tissue tilts downwards. The nipple and areola may also be stretched. If the dermis of the areola is thin, breast gland may herniate through the areola creating a prolaps of the nipple-areola complex.
In its mildest form, the breast may simply be slightly flattened in the lower half. Many forms exist, but it is useful to distinguish between those of normal volume (normovolemic type) and those with small breasts (hypoplastic type) where the gland is also underdeveloped.
The surgical options depend on how the shape and size need to be altered.
Normovolemic type
Hypoplastic type


Figure 1: Two different degrees of tubular breasts in the same patient. The right breast shows a moderate form with particular abnormality of the areola. The left breast is more hypoplastic with very limited developement of the lower quadrants. The left breast has a clear tube-like shape. |
Goals of the Surgery
The more complex forms of tuberous breast should be addressed in one or more operations. The skin of the lower part must be released and stretched. The areola may need reduction and/or lifting. Sometimes a simple breast lift is all that is required.
Surgical Technique
Three major steps comprise the approach to the tuberous breast.
Expansion of the breast base: this may be achieved in one visit with a fixed volume implant or may require the use of an expander. If an expander is used, the breast can be gradually stretched into shape and then exchanged for a permanent implant some months later.
Filling of the lower half of the breast: After expansion, or if the patient already has enough skin, the lower pole volume can be addressed. This can either be done with an implant or, in some cases, by moving tissue from elsewhere in the breast into this position. This leaves a scar around the nipple and a short vertical scar on the lower part of the breast.
Repositioning of the nipple: The areola may also need to be reduced during this process.
In the majority of patients, all three steps can be achieved through an areola incision.


Figure 2: (above) Mild presentation of bilateral tubular breasts. (below) Final result after expansion, permanent implant and lipofilling. |


Figure 3: (a) Severe bilateral tubular breast deformation. (below) Final result after conventional breast lift on the left breast and tissue expansion followed by lipofilling only in the right breast. |
What to expect after the operation
Dressings vary depending on the exact nature of the surgery. There will often be drainage tubes in both sides which can be removed after 1-2 days. Your recovery following surgery greatly depends on how extensive an operation was necessary.
Normal symptoms after surgery include:
Bruising
Temporary loss of sensation to the nipple, areola or surrounding skin
Swelling
Pain and discomfort
Restricted movement
Length of Stay
Minor corrections can be performed as day cases, whilst larger operations will require a stay of 1-2 days. A complete correction may need more than one procedure.
What to expect after discharge
If the wounds have been sealed with glue, the area can be showered the day afterwards. In other cases, you may have to wait for the wound to heal. Advice regarding bra use will be given on a tailored basis to taking into account the requirements of your operation. Sports and heavy work should be avoided for 4 weeks. Sleeping on your stomach should also be avoided during this time. It will be possible to do some normal housework within a few days
Potential Complications
Early:
Bleeding
Infection
Wound healing problems
Skin irritation
Late:
Permanent sensory loss in the nipple, areola or surrounding skin
Scar hypertrophy (thickening)
Asymmetry
Dissatisfaction with the final volume
Late effects of ageing
Implant problems (discussed in the augmentation section)
Financial Considerations
Tuberous breast is not a medical problem and does not cause any functional impairment per se. Depending on your health service or insurance, the operation may or may not be funded. It is important to clarify your funding status and the costs of the surgery with the surgeon and your insurer prior to surgery.
B. Volume Problems
The Small Breast
Every woman relates to the size of her breasts differently. There is no single ‘ideal’ which can encompass the multitude of cultural and environmental factors which create an individual’s attitude to her breasts. Thus, the ‘normal’ Asian breast is smaller than that found in Europe or North America, but within each of these societies, individuals will differ immensely in their perception of the ‘ideal’.
There is no medical issue with having small breasts (also known as hypoplasia). It is usually the woman herself who feels that her breasts are too small. Surgical treatment is aimed purely at improving the breasts appearance in the patient’s eyes.
The Large Breast
For the same reasons outlined above patients may feel that their breasts are too big over a broad range of actual breast sizes. Breast hypertrophy can, however, also lead to medical symptoms such as, skin irritation, back pain etc.
Surgical treatment reduces the volume, lifts the breast and reduces and moves the nipple and areola to a more aesthetically pleasing position.
The Sagging Breast
Again, this situation is defined by the perception of the patient rather than any hard-and-fast measurements. It is purely a cosmetic problem which can be defined as a patient who is happy with the appearance and volume in a bra, but is unhappy with the appearance without a bra.
Surgical approaches include reducing the skin and some of the volume to improve the shape.
Tubular breast
Tubular breast or tuberous breast is a more complex problem which has many variations. The lower part of the breast does not fully form and appears constricted by tight overlying skin. The fold under the breast can be shifted upwards and the remaining tissue tilts downwards. The nipple and areola may also be stretched. In its mildest form, the breast may simply be slightly flattened in the lower half. Many forms exist, but it is useful to distinguish between those of normal volume and those with small breasts where the gland is also underdeveloped.
C. Breast Asymmetry
Inequality between the two breasts can arise for a number of reasons. The disparity may be volume, shape or both. It can be very mild or quite pronounced. It can arise because of developmental changes affecting one or both breasts or the effect of age on one or both of the breasts. It is important to realise that no woman has completely symmetrical breasts and this is perfectly normal. The individual’s perceptions determine the point at which asymmetry becomes a problem. The most marked examples come as part of a recognised developmental problem such as tubular breasts, Poland syndrome or breast agenesis.
Surgical approaches use all of the techniques outlined in this website, choosing those which will give the patient their desired outcome. It is a highly personalized treatment and must follow clear and frank discussions between the patient and her surgeon. Surgery must be undertaken with a realistic expectation of what can be achieved. Also, patients must be aware that two or more visits to the operating theatre may be necessary.

Figure: mild to moderate asymmetry: the right breast appears normal but the left breast is slightly too large and more ptotic. |
D. Nipple Problems
Bi/trilobed nipple
In this condition the nipple forms in two or three parts instead of just one. Under local anaesthetic, the two or three parts can be released and brought together as one. There is some scarring and the resultant nipple can feel quite rough until this settles. Postoperatively the nipple is protected from pressure for 3-4 weeks.

Fig. 1

Fig. 2

Fig. 3
Fig1: a trilobed nipple before correction. |
Small or inverted nipple
An inverted nipple is one that lies flat or below the surface of the skin. It is caused by tightness in the ducts or surrounding fibrous tissue. In some cases, erection still causes the nipple to protrude, in more severe cases it does not. This condition would normally happen during puberty. Where the nipple goes from being normal to retracting, it is essential to establish that this is not being caused by a breast cancer. A mammogram may be requested prior to surgery.
The treatment has two components. The first brings the nipple back to its normal position. A small incision between the nipple and areola allows access to the ducts which can be loosened. If this is not enough, some of the ducts can be cut. The second stage aims to keep the nipple out while the scar tissue forms. The Niplette suction device may prove useful. A nipple piercing may be unacceptable in some social circles, but can be extremely useful in keeping the nipple out. It can be discarded after 1 to 2 years.
After surgery the nipple must be protected from pressure for 3-4 weeks. Scarring is minimal.

Fig. A

Fig. B

Fig. C

Fig. D
Figure: An inverted nipple (a, b) can be brought out and held in place by a nipple piercing (c, d). |
Oversized areola and nipple
This a purely cosmetic problem and opinions vary greatly as to what is the ideal size. There are variations between races and the only guide is what looks right for the individual. Approximately, for a Caucasian woman, an areola should be between 3.5 and 5.5cm.
Treatment can be performed under local anaesthetic. A doughnut of excess areola is removed. The resulting scar is very subtle as it is hidden along the edge of the areola. Healing takes approximately 2 weeks.

Hypertrophic nipple
Overly developed Montgomery tubercle (areola bumps)
In this condition, the pigmented sebaceous glands around the nipple can become dark or prominent. They can be removed surgically, but it is better not to be overly aggressive in their treatment.
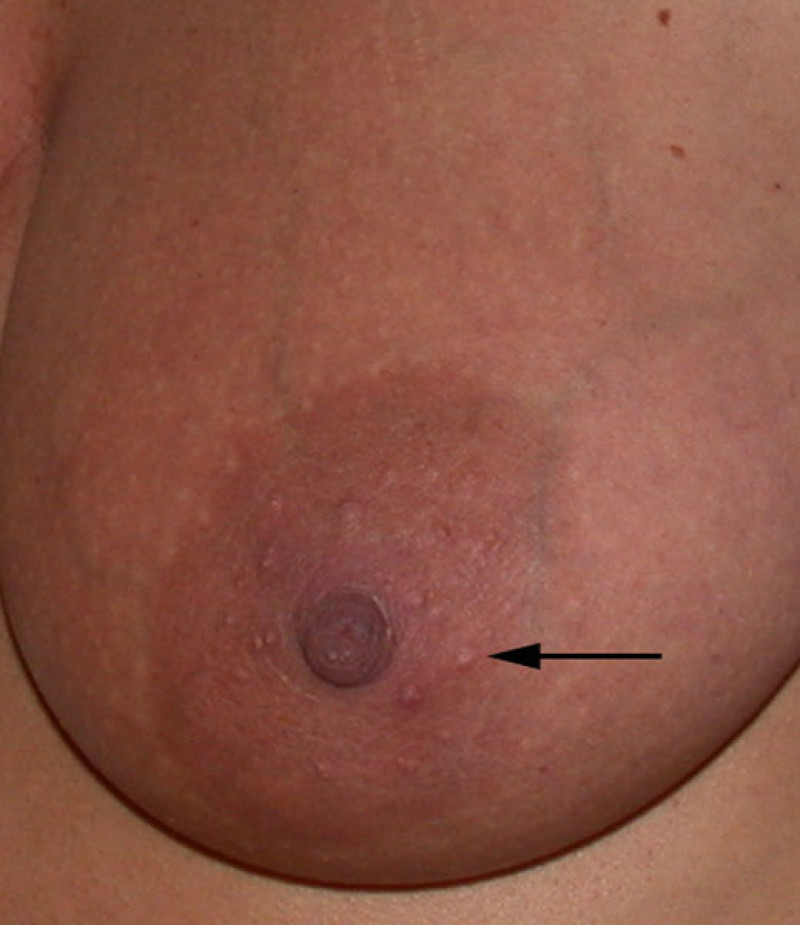
Montgomery tubercles (arrow)
E. Gynaecomastia
Description of the problem
Gynaecomastia is a condition that occurs in men, in which excess breast tissue forms behind the nipple. The volume may increase to such an extent that it may resemble a female breast and it can affect just one or both sides. This problem is essentially cosmetic, but can be very psychologically disturbing for the patient. There is however, no increase in the risk of developing cancer just because the breast tissue is larger.
The condition is quite common, affecting up to a third of the male population to some extent. The cause in the majority of cases is unknown. It happens because of sensitivity of the breast tissue to the hormones which circulate during puberty. An imbalance between male and female hormones occurs during puberty and also as testosterone levels dwindle in later life. Specific causes for gynaecomastia include congenital abnormalities, hormone-secreting tumours and some medications.
There is an important distinction in gynaecomastia between ‘true’ where the breast gland itself has caused the enlargement and pseudo-gynaecomastia where there is a general increase of fatty tissue in the area leading to the appearance of breasts. These two forms often combine.
The disease can appear as a slight bulge in the nipple region or go on to develop a fully formed breast. The condition can often resolve by itself, particularly where the underlying cause can be treated. If, however, the appearance persists, a plastic surgeon can help to remove the excess tissue.

Front view

Side left

Side right
Purpose of the procedure
If all underlying causes have been ruled out or treated and the disease has persisted for over a year, it is appropriate to proceed with surgical intervention. The goal of surgery is to remove the glandular tissu , excess fat and leave only a small scar under the nipple.
Surgical Technique
Fat and some of the glandular tissue can be removed by liposuction, but if residual glandular tissue still needs to be removed, this is done through a small scar along the lower edge of the nipple. After the gland has been removed, the excess skin can often be left to contract by itself, though it may initially appear wrinkled at first. Sometimes excess skin may also need to be removed. The tissue is sent to the pathologist to check for any abnormalities.


Figure: (above) Mixed type of gynaecomastia. (below) Partial gland resection combined with liposuction generates good results. |
What to expect after surgery
Sometimes a drainage tube must be left underneath the skin. This usually stays in for 1-3 days. Tight elastic bandage is used to compress the area after surgery. Some normal occurrences after the surgery include:
Bruising: especially after more extensive surgery
Temporary loss of sensation (chest and nipple)
Swelling
Mild pain and discomfort: The pressure bandage often worsens this, but it is an essential part of the postoperative care.
Restricted movement: partly caused by the bandage and partly by discomfort
Length of Stay
Mild forms can be treated as day cases, others may need to stay for 1-3 days
What can you expect after the surgery?
The elastic bandage needs to stay on for about 10 days. If the wound has been sealed with glue, the area can be showered after 3 days and the elastic bandage replaced. You are advised to restrict vigorous arm movements over the first 3 weeks. Hard work and sports are not advisable for the first 4 weeks. How long you feel uncomfortable for afterwards depends on the extent of the disease and your surgery.
Possible Complications
Local:
Bleeding
Infection
Wound healing problems
Skin irritation
Late complications
Permanent sensory changes
Asymmetry
Nipple flattening
III. Revisional surgery
A. Introduction
The popularity of breast surgery has significantly increased over the last 20 years. As the number of women who undergo procedures increases, so does the number of women who end up with a suboptimal result. Accordingly, a subspecialty has arisen within plastic surgery, aimed at patients who are unhappy with the results of their previous breast surgery.
Often, the basic techniques of breast surgery have not been applied. The plastic surgeon must therefore have extensive experience in order to adequately resolve problems that have been created. He or she may need to use the full range of breast reconstruction options in order to provide optimal patient care and achieve the best possible results.
Revisionary breast surgery poses a significant challenge for the plastic surgeon as large amounts of scar tissue may have formed and the anatomy may be distorted. The presence of scar tissue significantly alters soft tissue consistency. Therefore, although a second operation can produce a better result, it will often not be able to create a completely natural looking breast. It is very important that you discuss the surgical strategy with your surgeon and you understand what can be achieved by a further operation.
In this chapter, we will mainly discuss the management of late complications which arise after breast surgery. The chapter is divided according to the initial procedure performed, namely, breast augmentation, breast reduction, breast lift and breast reconstruction.
B. Revisional surgery following breast reconstruction
After implant
The same complications that were discussed in the section on breast augmentation can also occur in patients undergoing implant or expander based breast reconstruction. The most important complications are capsule formation and capsular contracture.
The main difference between patients undergoing breast augmentation and those undergoing a breast reconstruction following a mastectomy is that the skin envelope is often thin and less well perfused in the latter group. Patients who require radiotherapy following an implant reconstruction, frequently rapidly develop severe capsular contracture.
Although capsular contracture, implant displacement and implant rupture can usually be corrected by replacing the implant or by the use of expanders, it is generally advisable to remove both the implant and scar tissue and perform a reconstruction using the patients’ own tissue.
Complications following implant reconstruction can present in very different ways and it is therefore difficult to describe the best surgical solution for each individual patient. You should contact your plastic surgeon and discuss the possible options. A combination of the techniques described in the chapter on breast reconstruction can be applied to achieve a good aesthetic result.

Fig. A

Fig. B

Fig. C

Fig. D
Figure 1: (a) result after repeated attempts at breast reconstruction using implants. The patient had radiotherapy on the right side before the implant was removed. On the left side the implant has been distorted by severe capsular contracture. (b,c,d) Result after removal of both the implants and scarred tissue and bilateral free DIEAP flap breast reconstruction, including nipple reconstruction and tattooing of the areolae. |
After Autologous
The early and late complications following autologous breast reconstruction were discussed in the chapter on breast reconstruction. It usually takes two to three operations to achieve the final result and therefore most minor problems can be adequately treated during these subsequent procedures. Once the tattooing has been finished, further revisions are rarely necessary.
The main advantage of using one’s own tissue for reconstruction is that it appears natural and lasts a lifetime. However, late complications may arise, although this is unusual. Tattoos do fade though and it may be necessary to re-tattoo the areola at some stage.
Even though abdominal muscle is not removed, or only a small amount is sacrificed, weakening of the abdominal wall muscles where the flap was dissected can occur. However, this is extremely rare. It usually results from stretching of the connective tissue layer of the abdomen or because of suture rupture. If the problem is severe or if it causes functional disturbances, your plastic surgeon must strengthen the connective tissue layer in the abdomen and can gain access through your existing scar.
Breast reconstructions are also subject to ageing, just like any normal breast. Surgical procedures to improve breast shape can also be performed on reconstructed breasts. Additionally, weight fluctuations will cause fluctuations in breast size. In contrast, if an implant reconstruction was selected, the breast volume does not vary. If weight fluctuations do occur, progressive asymmetry between the two breasts may result. The asymmetry is less pronounced in patients who have had reconstructions using their own tissue. One should always remember that the tissue used is usually from the abdomen or the buttock and therefore is more sensitive to hormonal changes than a normal breast. In cases where the asymmetry is very significant, surgery can be performed to either the reconstructed or the normal side.
The small percentage of patients whose previous implant reconstruction or autologous reconstruction failed, can opt to undergo a secondary reconstruction. This can be performed using a new implant, a pedicled flap from the back or a new free flap from the buttocks or the abdomen. However, before embarking on a second procedure it is very important to try and understand why the first procedure failed. Patients who suffer from, for example a coagulation disorder and that led to the flap failure, are excluded from any further microsurgery. However, in most instances a second free tissue transfer can be performed with no greater risk of complications than for the first procedure.
Finally, one should remember that breast cancer can recur and that a new tumor can develop in the reconstructed breast. Although during a mastectomy most of the glandular breast tissue is removed, it is impossible to completely remove all the cells. Any residual cells may produce a further tumour requiring additional surgery. Each patient must therefore be assessed individually to determine how much tissue should be excised and which type of reconstruction should be performed. This should be a combined decision after discussion with your plastic surgeon and the oncologist.
After Breast Conserving Surgery
Patients who undergo conservative surgery and radiotherapy followed by breast reconstruction are at risk of late complications. Most importantly, careful monitoring for recurrence and the development of new tumors in the remaining glandular tissue must be regularly performed. In addition, there is a risk of the potential sequelae of radiotherapy. As is the case following a full mastectomy, a recurrence or new breast tumor may develop after conservative surgery. If it is not possible to perform a local resection, removal of the entire breast, including the partial reconstruction should be performed. In this case one would apply the conventional techniques of breast reconstruction which have already been described.
A specific problem which usually results following conservative surgery and radiotherapy is fibrosis and scarring of the remaining glandular tissue. Radiation injuries can appear 15 to 20 years later. However, most changes occur during the first two years. Deformity of the breast may lead to a significant alteration in the shape and volume of the breast which may necessitate further surgery. A decision must be made regarding which breast to adjust. As before, the techniques used in breast reduction, breast augmentation and breast lift can all be applied. It is important to do as little as possible to the irradiated areas, as wound healing tends to be a problem.
If scarring and fibrosis is severe it may be necessary to remove the entire breast and reconstruct it using one of the previously described techniques.
After nipple reconstruction
A nipple reconstruction may flatten due to changes in volume or secondary to the ageing process. Typically, the nipple loses projection after a few years. A short and simple operation can enlarge the reconstructed nipple. Additional tattooing of both the nipple and areola is then also required. Tattoos tend to fade anyway and often have to be repeated several years later.
Poor positioning of the nipple and areola is usually a result of bad pre-operative planning. Sometimes, the position of the nipple may be altered by scarring or the side effects of radiotherapy. If the areola is displaced too far from its natural position and cannot be simply repositioned, the nipple reconstruction may have to be abandoned and started over again in the correct location.
C. Revisional surgery following breast augmentation
Introduction
Early complications following breast surgery are described in the chapter on breast augmentation. Even though these can easily be treated, complications such as infection or secondary haemorrhage can significantly increase the long term risk of capsular contracture. The treatment of capsular contracture and other late complications are discussed.
Capsular Contracture
A capsule is always formed around an implant, regardless of whether the implant has been used for breast augmentation or for breast reconstruction. Initially, the capsule is thin and flexible. Over time, the capsule may become thicker and eventually contract. The reasons for this remain unclear but the phenomenon is called capsular contracture.
Contraction of the capsule around an implant may cause it to become deformed and can lead to chronic pain and a feeling of tightness in the breast. Capsular contracture can occur just a few months after the placement of an implant, but equally it may occur later, even after 20 or 30 years.
Once capsular contracture becomes uncomfortable for the patient, she may wish to consider a revision. In most cases, either a capsulotomy or a capsulectomy is performed.
In a capsulotomy, the implant is removed through the existing scar and incisions are made in the capsule, in different directions, so that the surrounding tissue can re-expand. The breast implant may then be replaced.
In a capsulectomy, the entire capsule surrounding the breast implant and the implant itself are removed through an incision in the fold of the breast. Once again, the breast implant may be replaced or exchanged for a new one.
Implants may have to be removed if severe capsular contracture recurs in the same patient or if the patient chooses this option. In these cases, it may be necessary to perform a breast lift (mastopexy) because the overlying skin and breast tissue have been stretched over a long period of time. Otherwise, the breast support has been lost and the soft tissue droops.
Depending on the patient’s wishes, it is also possible to create a new breast using reconstruction techniques and the patients’ own tissue.

Fig. 1a

Fig. 1b

Fig. 1c

Fig. 1d

Fig. 1e

Fig. 1f
Figure 1: (a) unilateral capsular contracture with displacement and deformity of the left breast. (b, c, d) Postoperative images following capsulectomy and implant exchange. (e, f) The capsule compresses the implant causing rippling. After releasing the thick capsule, the implant shape is restored. |
Rotation of an implant
Rotation of an implant most frequently occurs in the first post-operative week. This problem only affects anatomical implants. It is important to apply dressings to the upper part of the breast after surgery so that the implant integrates and becomes fixed in an ideal position. However, if the implant does become integrated, it may still move or rotate within its pocket for months or even years following surgery.
If rotation of the implant does occur, the breast will quickly develop an unnatural shape, with the upper pole gaining more projection than the lower pole. Contraction of the pectoralis major muscle can cause the implant to move. In the early postoperative period, it will primarily move upwards, whereas later in the post-operative period it tends to move downwards and outwards. This may result in significantly asymmetrical breasts.
Displacement or rotation of the breast implant can only be resolved surgically. After removal of the implant, the pocket must be corrected accordingly. In some cases it is necessary to remove or close part of the capsule. Frequently, the solution is to move the implant from in front to behind the pectoralis major muscle, or vice versa.
If an implant has migrated downwards due to surgical disruption of the inframammary fold, the fold has to be recreated and then the implant can be exchanged.
Ruptured Implants
This complication is more common in women with saline-filled implants than with gel-filled implants. Late rupture usually occurs because of weakness of the outer layer of the implant. Small folds may form on the implant when it is inserted. The corners of the folds cause continuous friction as a result of everyday movement. After several years, the implant may then develop tears at the site of these folds.
Implants that have been in place for a long period of time can rupture spontaneously. Sudden external trauma can also damage an implant, although this is rare.
A ruptured saline implant deflates within 24 to 72 hours. This poses no threat to the patient because saline is completely removed by the kidneys. However, the aesthetic impact can be significant and prompt exchange of the implant is recommended. If one waits too long, the capsule will continue to contract and a more complex procedure will be required to re-insert a new breast implant.
Arrival of the new, cohesive, silicone gel-filled devices has resulted in much fewer serious complications following implant rupture. The liquid gel which was used in the past migrated into the surrounding tissues after rupture. Many patients developed serious complications as a result of this.
With the new gelatine-like silicone implants, the gel remains in situ even if the outer layer ruptures. As a result, with these new implants a rupture may remain asymptomatic for a long period of time, only becoming problematic when capsular contracture develops. A capsulotomy and implant exchange solves this problem.
Skin necrosis
This is rare but predominantly occurs in patients who opt for very large breast implants and have thin overlying skin. The constant pressure on the lower poles of the breasts due to the effect of gravity, leads to progressive narrowing of the blood vessels. This causes the skin to necrose and later perforate.
Once the skin perforates, the implant is exposed and there is a high risk of infection. The surgeon must therefore remove the implant, thoroughly disinfect the cavity, close the skin defect and insert a much smaller device. In some cases it may be advisable not to replace the implant.
Assymetry
The goal of breast surgery is to achieve symmetry. A patient should understand that a small amount of asymmetry is normal. Women do not naturally have perfectly symmetrical breasts. Breast asymmetry, therefore, also applies to women who have had breast surgery and in fact, breast asymmetry may be more pronounced following surgery. There may be a disparity in shape, volume, position or orientation of the breasts. If a patient has a degree of asymmetry pre-operatively, this asymmetry will still be present following breast augmentation, although it may be less noticeable. Patients who have a marked volume disparity prior to surgery may have two different sized implants inserted.
Exceptional differences in breast sizes must be corrected using very specific techniques. This will vary with each patient and is best discussed with one’s plastic surgeon.
Distance between breasts
The position and distance between breasts varies significantly amongst women who have not had breast surgery. Equally, nipples may also be far apart and it is difficult to perform a breast augmentation that will correct this. Placing an implant in front of the pectoralis major muscle often brings the nipples closer together. If both nipples are oriented outwards, it is sometimes necessary to use very large implants in order to achieve naturally looking breasts. In some cases, it is impossible to correct the distance between the breasts and a patient may have to accept this.
Lipofilling may be able to smoothen out the transition between both breasts.
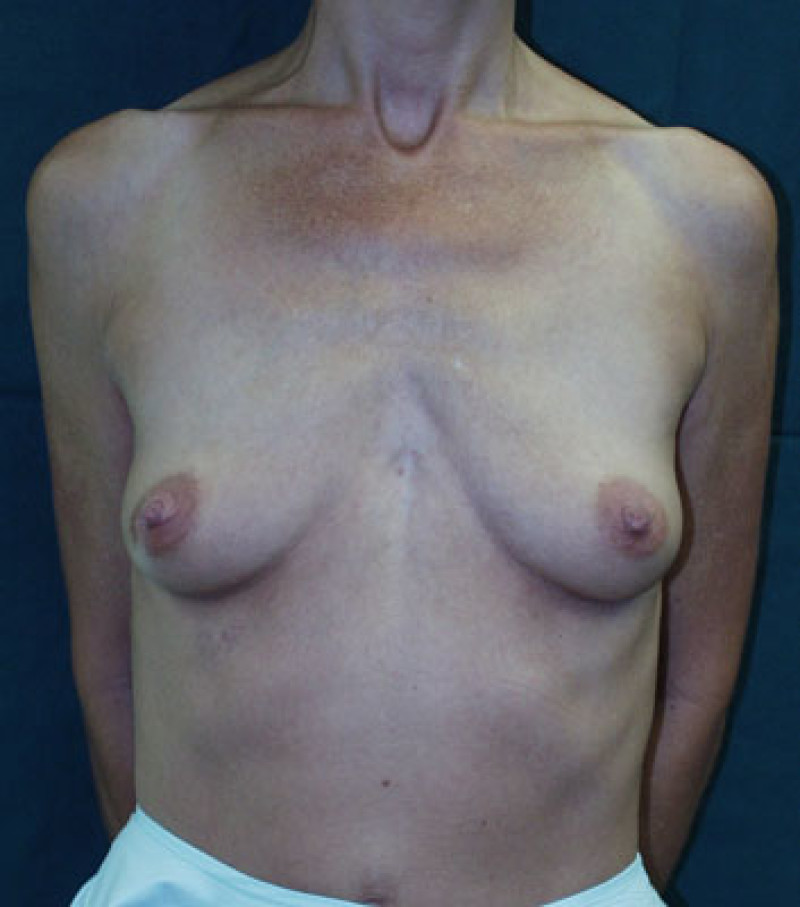
Fig. 2a

Fig. 2b
Figure: Pre-operative image (a) and postoperative image (b) of a breast augmentation in a patient with an increased distance between the two breasts. This distance cannot be reduced unless very large implants are inserted. |
Dissatisfaction
Before undergoing a breast augmentation, the patient and the plastic surgeon discuss the patients’ desired breast volume. The breast volume is estimated using a trial implant, chosen by the patient pre-operatively. Although this is routinely performed, occasionally a patient may feel that the augmented breasts are still too small following surgery. This problem can only be resolved surgically. If the patient wants larger breasts, the current implant is removed and a larger implant inserted. This is performed through the same incision. At the other extreme, a patient may feel that her implants are too large. This is very rare but again can only be resolved by exchanging for smaller implants.
D. Revisional surgery following breast lift
The commonest complaints from women who have undergone breast lifts are asymmetry and recurrence of sagging in the long term.
Pronounced asymmetry between both breasts after a breast lift is usually due to poor pre-operative planning. Asymmetry of the shape and position of the nipple and areola can usually be addressed using the existing scars.
Fluctuations in weight and ageing can also affect the quality of the surrounding skin, so that the breasts begin to sag again. This problem can also be corrected using the existing scars and a short procedure.
E. Revisional surgery following breast reduction
Nipple-areola complex (NAC)
Circulatory disorders affecting the nipple and areola are rare but may cause a significant deformity in this area of the breast.
Blistering and crusting of the areola occurs if the lack of blood supply is temporarily reduced. The wound usually heals spontaneously but tends to leave an area of scar tissue which contains less pigment.
Once the scar has fully matured and if the basic structure of the nipple and areola has been preserved, this area can be tattooed, to restore the natural appearance of the areola.
If the blood supply is severely impaired, the nipple and areola may necrose. In this instance, the cosmetic deformity is much worse. The necrotic skin has to be excised and the healthy wound closed with stitches.
Once the scar has matured, nipple reconstruction can be performed
Breast tissue
This complication is extremely rare but has serious consequences.
Patients with a pre-existing vascular disorder and those in whom the wrong surgical technique is employed are at significant risk. A portion of their breast tissue may die and become infected following surgery. This can lead to abscess formation or a cutaneous fistula.
If large areas of the breast are involved, a significant loss of volume and extensive scarring may result.
In smaller areas, fat necrosis can occur. An area of breast tissue is transformed into a hardened mass, consisting of oil mixed with small cysts.
On palpation, an area of fat necrosis feels similar to a malignant lesion, although fat necrosis is an entirely benign process. However, it may cause confusion during mammography.
The treatment of fat necrosis varies. Small areas can be monitored but large areas may have to be surgically excised, if the wounds break down or tissue becomes infected.
Ideally, it is useful to wait, possibly for several months, to determine which areas of the breast tissue will recover.
If large areas are excised, it may be necessary to consider autologous breast reconstruction.
Scarring
Scars positioned on the lower part of the breast usually heal very well. The length of the scar tends to be proportional to the amount of breast tissue removed; the larger the breast reduction, the longer the scars.
Hypertrophic scarring occurs when excess scar tissue forms. The scar typically becomes red, raised, firmer and wider. This can be distressing for patients but is often genetically determined.
Hypertrophic scars are initially treated by regular massage and the application of pressure. This can be combined with a series of intralesional cortisone injections. In severe cases of hypertrophic scarring, surgical excision followed by local irradiation may be necessary.
Excess skin can sometimes gather at the lower aspect of the vertical scar or at both ends of the horizontal scar. This is known as a ‘dog ear’. These can be surgically excised if they are very prominent or if a patient finds them uncomfortable or unsightly.
Finally, all scars may stretch and become wider, warranting surgical revision to improve their appearance.
Assymetry
As with all breast operations, a small amount of residual asymmetry is inevitable, as no two breasts are entirely identical.
Any asymmetry may be related to the breast volume or shape. If there is a volume difference, this can be corrected by reducing the larger breast or by augmenting the smaller breast. The breast shape can be improved by resecting limited amounts of skin or by moving the position of the nipple/ areolar complex.
If the nipple/ areola complex ends up being positioned too high or too low on the breast mound, it reflects poor pre-operative planning. An areola that is too low can easily be corrected, using the same scars that were used for the breast reduction. However, an areola that has been placed too high is a much more difficult problem to correct. Lowering the areolar can leave significant scars that are visible when wearing a bikini or low cut top.
Nipple retraction
Nipple retraction may also occur following breast reduction surgery. The scar tissue that forms underneath the nipple/ areola complex can cause the nipple to be pulled inwards. This usually occurs due to the influence of gravity on the healed glandular tissue. Nipple retraction is however, surgically correctable.
Volume shape
Massive weight loss patients tend to lose a significant amount of glandular tissue, however, the surrounding skin does not change. As a result, the breasts tend to sag and lose projection.
A patient may opt to have the breast volume increased and this can be achieved using standard augmentation techniques. Alternatively, a breast lift may be performed to improve the breast shape.
Conversely, patients with significant weight gain tend to increase their breast volume. These patients may opt for a secondary breast reduction, which can be performed through their previous scars.
It is important that patients who are prone to weight fluctuations achieve a stable weight, which should be maintained for at least one year, before undergoing further breast reduction surgery.
As a result of the natural ageing process, the breast envelope can lose elasticity and firmness. It is especially common in the lower part of the breast, which is the area most effected by gravity. This results in an unattractive shape, where the areola remains in place, but the glandular breast tissue descends towards the lower pole of the breast. This deformity is particularly common after a vertical scar breast reduction.
It occurs because insufficient skin was removed from the lower pole of the breast at the first operation. In order to correct this, the glandular breast tissue needs to be reshaped and positioned higher. This can be done through the existing scars but often, it is also often necessary to excise skin at the lower poles, both horizontally and vertically.

Fig. 1a

Fig. 1b
Figure 1: Pre-operative picture (a) of a breast reduction patient, in whom the nipple-areolar complexes were positioned too high on the breasts. Post-operative picture (b) demonstrating corrected nipple heights. The scars above the areolas are inevitable. |
