Prevention
Modern medicine is increasingly transitioning towards preventive care. This shift towards prevention has also been observed in breast cancer care in recent years, particularly with the discovery of the BRCA gene. Subsequently, multiple genes and risk factors have been identified. Depending on these factors, a personalized screening strategy can be chosen. Therefore, it is crucial to understand these genetic and risk factors.
Diagnosis
I was diagnosed with cancer ... This website serves as a portal designed to assist you and your loved ones in accessing personal information and finding solutions to your concerns.
The primary goal of this website is to offer guidance and support to patients as they navigate their journey toward recovery and improved quality of life. The "Diagnosis" section of our website is divided into two main categories. Firstly, under "Anatomy and Physiology," we provide fundamental knowledge about the breast. Secondly, in the "Tumors and Disorders" section, we delve deeper into various breast-related conditions.
Moreover, we aim to provide information to women who may be concerned about potential breast issues but are hesitant to seek immediate medical advice. Knowledge and information can often offer immediate reassurance if a woman is able to identify the issue herself and determine that no specific treatment is necessary. Conversely, we also strive to educate women who have received a diagnosis of a serious breast condition, such as breast cancer, and wish to approach their doctor well-informed and prepared.
Treatment
The treatment for breast cancer should immediately include a discussion about reconstruction. Our foundation has no greater goal than to raise awareness of this among patients and oncological surgeons. By making an informed decision beforehand, we avoid closing off options for later reconstruction while still considering the oncological aspect. Of course, survival is paramount, and the decision of the oncologic surgeon will always take precedence.
The "Reconstruction or not?" page contains all the information you can expect during an initial consultation before undergoing tumor removal. This page is comprehensive, and your plastic surgeon will only provide information relevant to your situation.
"Removing the tumor" details the surgical procedure itself. This is the most crucial operation because effective tumor removal remains paramount. We guide you through the various methods of removal, a decision often made by a multidisciplinary team comprising oncologists, radiologists, pathologists, radiotherapists, breast nurses, gynecologists, oncological surgeons, and plastic surgeons.
The "Breast Reconstruction" section includes information and illustrations of the different reconstruction options along with corresponding steps.
Revalidation
Those treated for cancer often need a long period to recover.
Cancer is a radical illness with a heavy treatment. Often, people have to deal with psychosocial and/or physical problems afterwards, such as stress, anxiety, extreme fatigue, painful joints, reduced fitness, lymphedema... This can have a major impact on general well-being.
There are rehabilitation programmes offered by most hospitals. We cover some of the major topics here.
Quality of life
Quality of life is a key factor in coping with breast cancer. Therefore, it is important to find coping mechanisms that work, which will be different from patient to patient. For some, it may be finding enjoyment in activities they engaged in prior to diagnosis, taking time for appreciating life and expressing gratitude, volunteering, physical exercise... Of prime importance, studies have shown that accepting the disease as a part of one’s life is a key to effective coping, as well as focusing on mental strength to allow the patient to move on with life. In this section we are addressing some topics that patients experience during and after treatment and we are providing information to address them.
Anatomy and Physiology
Anatomy is a branch of science that describes the structure of living beings. We describe here the normal structure of the breast in order to have a basic knowledge when you visit the doctor. This basic knowledge will also help you to understand some breast diseases and interventions.
Physiology is a branch of science that will describe the same structures but on a cellular level. Because the cause of many problems starts at the cellular level, it is important to have some basic knowledge of this too.
Anatomy
The normal appearance of a breast
What does a normal breast look like? Watch the following video by Laura Dodsworth:
Development of the breast
During fetal development, the breast first arises as a pigmented nipple elevation of the chest skin, on each side of the sternum. The breast ducts are formed by an invagination of these nipples. The milk duct structure and the nipple of the breast are present at the time of birth.
The breast glands develop during puberty under the influence of hormones. During this period, they are also surrounded by more fat which contributes to the final adult volume and shape.
During pregnancy, the glands are temporary activated to produce milk by hormone stimulation.
During menopause the breasts atrophy and decrease in volume.
Structure of the breast
In the anatomical position, the female breast lies at the level of the second to the sixth rib. The breast covers a large part of the pectoralis major muscle. The breast can be considered in terms of its volume and its skin envelope. The skin envelope is partly responsible for the shape of the breast.
The nipple and areola are important features at the ‘top’ of the breast. Both contain pigments. The areola is usually round. The nipple is located centrally in the areola. Randomly distributed around it, small pale coloured bumps can be found called Montgomery glands. They produce sebum. In some circumstances, they may lead to a cyst.
The female breast is composed of approximately 15 to 20 lobes. Each lobe is made up of many smaller lobules where under certain hormonal conditions milk can be produced. The milk duct collects the milk from the lobules and carries it to the nipple. The lobes are embedded in adipose tissue and are separated by fibrous membranes which are attached to the underlying muscle, holding the entire structure together. These fibrous membranes are the ligaments of Astley Cooper. Together the skin, the adipose tissue around the glands and the glands themselves, determine the overall shape of the breast.
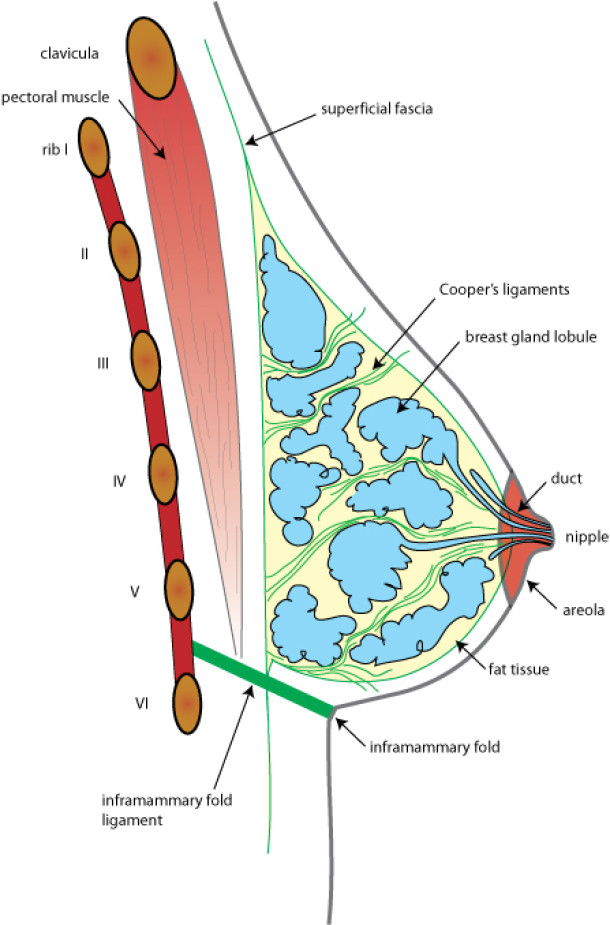
Fig. 1. Composition of the breast: glandular tissue (blue), fat (yellow) and connective tissue strands (green) are contained between two sheets of the superficial fascia, a tough connective tissue layer that surrounds the entire body. A strong ligament determines the position and shape of the inframammary fold. The chest is separated from the underlying pectoralis major by a network of loose connective tissue.
Blood supply of the breast
The breast has a rich blood supply from a number of different sources. The main supply is from an artery that originates in the armpit. There is an additional supply from both the internal throracic arteries (originating near the sternum) and from the arteries of the ribs.
Drainage is through a network of veins which follow a similar pattern to the arteries and, additionally, through a complex framework of superficial veins just under the skin. Many of these veins are visible to the naked eye.
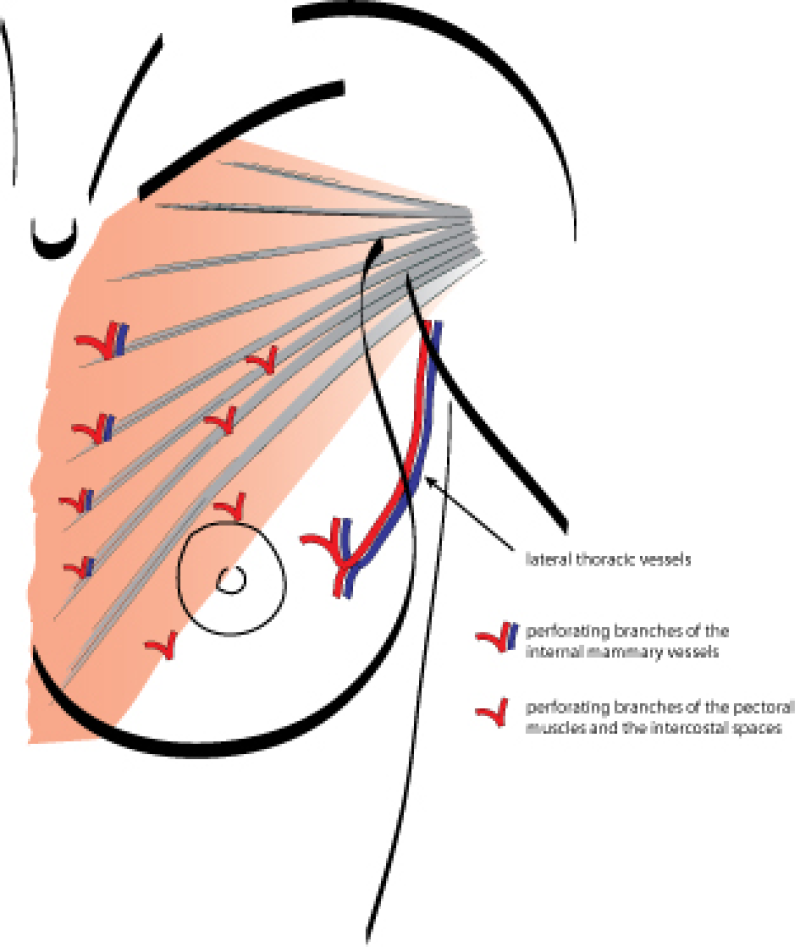

Left: blood flow in the chest: arteries (red) and veins (blue) create an extensive network of blood vessels. | Right: typical appearance of the superficial veins in the breast. |
Lymphatic drainage
The lymphatic drainage of the breast is an equally large network and plays an important role in breast cancer. Much of the lymph is drained from the outer chest wall to the lymph nodes within the armpit (approximately 20 to 30 ‘axillary’ lymph nodes). The remaining lymph is drained towards the midline, to the lymph nodes in the region of the sternum (parasternal nodes). The two axillary lymph node regions are connected with each other via a lymphatic network across the chest. The lymph then flows from here to beneath the collarbone and the base of the neck. There is a direct connection to the large veins that run back to the heart. In some rare cases there is also direct drainage to the mediastinum, liver, parasternal and axillary lymph nodes from the other side and along the ribs.
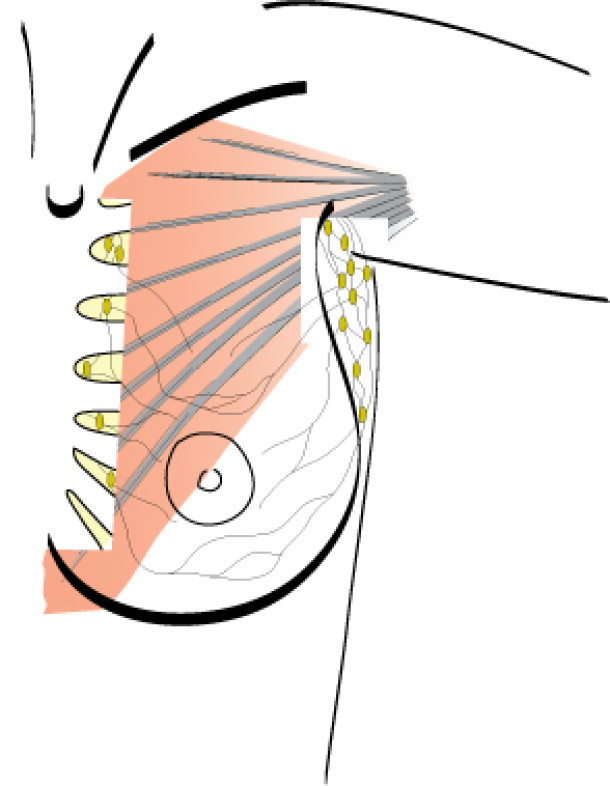
Fig. 3. Lymphatic drainage of the breast: Lymphatic fluid is drained to the axilla and the parasternal nodes (lymph nodes along the sternum) through a complex network in the breast and subcutaneous tissue.
Innervation
Sensation to the breast skin is supplied by nerves that run horizontally from the sides towards the center of the chest between the 2nd to the 6th ribs. The nerve at the level between the 4th and 5th rib is especially important as it provides sensation to the nipple and areola. The upper areas of the breast are innervated by superficial nerves coming down from the base of the neck.
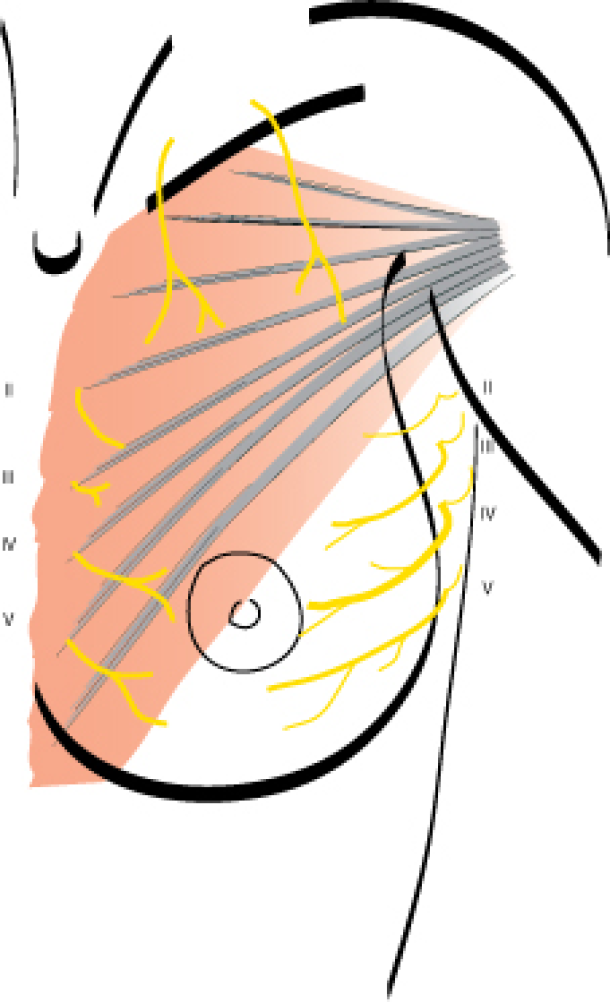
Fig. 4. Sensory nerves of the breast: the most important nerves follow the intercostal spaces II to V, both along the sternum and from the flanks. The IV lateral intercostal nerve is the most important nerve for the nipple and areola, as well as for erogenous sensitivity.
Physiology of the breast
Puberty
The breast is a gland common to both males and females. Men only have glandular tissue confined to the nipple and areola. This is also the case for girls before puberty, but during puberty this glandular tissue enlarges considerably.
Puberty lasts 4 to 5 years in girls and follows a similar pattern. The first stage is called the ‘growth spurt’ where growth is accelerated. Next comes early breast development: the areola increases in diameter and the areola and nipple protrude from the chest. On average this happens before the age of 10.
About nine months later, further development occurs alongside that of the pubic area. The hair near the armpit is visible two years later. The first menstrual bleeding occurs around the average age of 12.8 years. There is a range in age when girls experience their first period: some as young as 9 years old; others can pass the age of 17 before they experience menstruation.
Next the breast volume increases. The change in shape and volume of the breast is due to an increase in the gland tubules, adipose tissue and the supporting tissues of the breast. The mammary gland is usually fully developed around the age of 14 to 15 years.
After puberty, the extensive system of ducts increases. During each menstrual cycle, the number of channels increases. In addition, these channels also continue branching. If you cut through the channel and view it under a microscope, (Fig. 1), a hollow tube surrounded by cells that are neatly arranged next to one another can be visualized. These cells are called epithelial cells. Around these are smooth muscle cells surrounded by a thin membrane (Fig. 2).
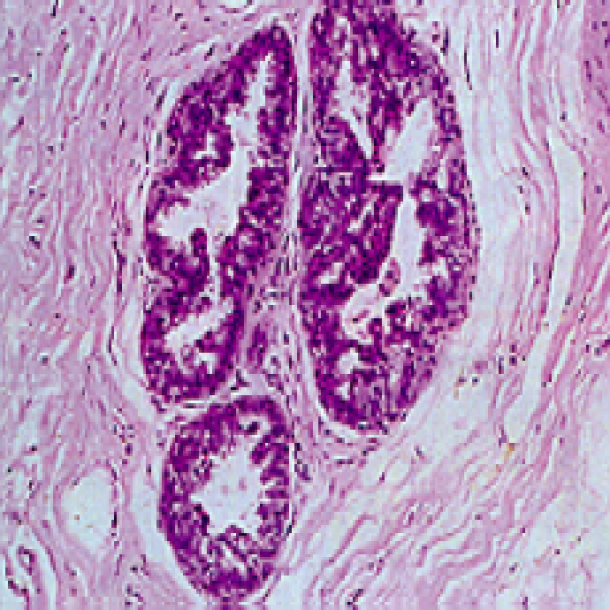
Figure 1: Transverse section through a breast duct as seen under a microscope
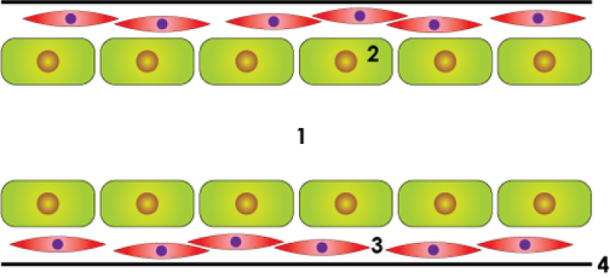
Figure 2: Schematic representation of the milk duct: lumen or central cavity (1), epithelial cells (2), smooth muscle cells (3), thin membrane or basal membrane (4).
The breast in pregnancy
During pregnancy, there is a visible increase in breast size. A rapid increase in breast volume may also be due to an overall increase in weight. There is an increase in the branching of the breast ducts. Additionally, there is an increase in the number of breast gland cells in the ducts. The breast cells gradually accumulate ‘colostrum’ fluid. This ‘colostrum’ will be released after delivery and contains many proteins. After one to three weeks post partum, the flow of colostrum ceases.
The shorter the period between the first menstruation and the first full-term pregnancy, the lower the risk of breast cancer. The exact mechanism of the beneficial effect of pregnancy (before 30 years of age) in the mammary gland is still unknown. The majority of cells in the breast ducts produce milk under the influence of pregnancy. This leaves fewer cells to control cell division and development of new cells. Although these latter cell types are needed to replace breast cells, they are also prone to transformation into cancer. The more limited their number, the less the chance of breast cancer. After pregnancy and / or after discontinuation of breast-feeding, the mammary gland returns to its normal volume.
Taking birth control or using an intrauterine hormonal device (IUD) will not affect the risk of breast cancer. In a normally menstruating woman, taking birth control pills will have virtually no influence on the appearance of the breast, especially when a low dose oral contraceptive is taken. For many women with premenstrual breast tension, the pill will even give an improvement in symptoms.
Breast feeding and breast surgery
The number of breast operations continues to rise as more and more young women have corrective breast surgery. Due to the development of late complications and the natural aging process, one or more re-operations will be required in up to 20% of these women within a few years.
A significant proportion of these women are in the fertile phase of their lives, which means they may choose to have children in the period following surgery. Surgery always leaves scars and this affects the ability to breastfeed after giving birth.
Potential complications resulting from the operation should always be discussed with the patient. These include the presence of scars and the process of scar maturation, the possibly altered sensation to the breast and nipple and the implications for pregnancy and lactation. Operative techniques can be adapted for women who wish to become pregnant and breastfeed. They may be advised to postpone surgery if uncomfortable with any of the potential adverse effects.
Generally speaking, breastfeeding is still possible after corrective or aesthetic surgery of the breast. This is clearly dependent on the exact type of operation. Extensive surgery and multiple operations will inevitably make the possibility of breastfeeding less likely, especially if the feeling in the breast and nipple / areola is absent.
Below is our advice for postoperative breastfeeding according to the procedure performed:
1. Breast augmentation
In this procedure, the breast is enlarged using a silicone implant. The implant may be placed on or behind the pectoral muscle. Most women can breastfeed after a breast augmentation.
The amount of milk that can be produced is directly related to the amount of glandular tissue but not to the absolute size of the breast itself. A small breast with a lot of glandular tissue may produce more than a large breast with a small amount of gland.
Problems can occur when a scar around the areola is made. In this approach, the milk ducts and nerves are cut, with the resulting negative consequences on breastfeeding. The feeling in the nipple may also be reduced.
When the volume of the breast prosthesis is large (especially when placed on the pectoral muscle), the prosthesis exerts so much pressure that the breast tissue scars and shrinks, with inevitable consequences.
Often women who have undergone breast augmentation with silicone implants are concerned that the silicone might contaminate the breast milk. However, research has shown that this is not the case.
After a breast augmentation capsular constracure may occur around an implant. If this is very extreme, reoperation is necessary, with potential increased scar formation and damage to the breast tissue, thus adversely affecting future breastfeeding.
When lipofilling (injections of fat) is used to increase either a portion or the entire volume of the breast, fat is injected behind the gland and between the skin and gland. In this way the gland itself is not affected and there will be no interference with breastfeeding.
2. Breast reduction
This procedure is performed for women who have large breasts that cause functional problems, such as back, neck and shoulder pain. There are several techniques for this operation, but in general the nipple and areola are moved upwards and tissue is cut away at the bottom and / or centrally in the breast. The scars are around the areola, vertically downwards from the areola and usually horizontally in the crease underneath the breast.
Even after a breast reduction, most women can successfully breastfeed, although this is dependent on the surgical technique. Today’s sophisticated procedures result in less damage to the nerves of the breast and the milk ducts. The duration of breastfeeding is however often shorter than in women who have not undergone surgery. It is also possible that the amount of milk is insufficient for the baby and that additional bottle feeding may be required. Problems are particularly likely in women where a lot of breast tissue was removed during surgery and where there is reduced or no nipple sensation.
In patients who get a postoperative wound infection, scarring may occur in the breast with additional consequences.
Some women who have undergone breast reduction, are frightened to breastfeed because they fear that this may have an adverse effect on the shape of the breast, but this is not true.
3. Breast lift
In a breast lift, the breasts retain their volume but the nipple and areola are returned to a ‘normal’ position. Technically this is done only by removing excess skin in order to re-shape the breast.
Often breasts are weakened due to the aging process or after pregnancies and / or weight loss. Many of these women are unconcerned about the ability to breastfeed, but generally, in comparision to a breast reduction, the breast tissue and nipple areola are unlikely to be damaged in this type of surgery and therefore breastfeeding remains possible.
4. Correction of congenital breast abnormalities
The exact cause of congenital breast abnormalities (abnormalities in the breast from birth) is unclear. In an extreme case, the breast is not formed. At other times, one or both breasts may be tubular in shape (see also Developmental Disorders of the breast).
For psychological reasons, correction is highly desirable and often started at a younger age (around puberty). Breastfeeding in a deformed breast may result in problems and is sometimes impossible. There is too little or no breast tissue and surgery may cause further damage or adverse consequences. If the other breast is unaffected this may be used to breastfeed.
5. Breast reconstruction
This term is used in women who have had breast cancer, when part or all of the breast has been removed and a reconstruction has been performed. Logically, breastfeeding is not possible afterwards.
Any further pregnancy in breast cancer patients also results in an increase of female hormones in the bloodstream with a concomitant increased risk of developing new tumors, recurrences or metastases.
The influence of the menopause and hormone replacement therapy on the breast
The onset of the menopause typically occurs at 52 years. After that, few sex hormones are produced by the ovaries. Hormonal stimulation in the breast tissue decreases. This disappearance of the female hormones can cause problems which can be divided into short and long term;
The most recognizable problems in the short term are the vasomotor symptoms. 60% of women experience flushing, problems with irritability and poor sleep. These symptoms can be very social disabling.
In the long term, loss of hormone production can cause bone mineral loss and osteoporosis. In later life, this may result in fractures of the vertebrae, hips and wrists. The skin of the vaginal lining becomes thin and brittle. This may cause pain during intercourse. The lining of the bladder may also become thin, leading to incontinence. There is a clear link between the loss of hormone production and dementia.
The loss of sex hormones results in a regression of the glandular tissue of the breast. The breast tissue contains more primitive glandular tubes again, while the highly branched glandular tubes decrease in number. Other women in the menopause clearly gain weight. The fat accumulates mainly in the abdominal wall. An increase in body weight may also increase breast volume.
Women with menopausal symptoms (hot flushes, sweating, poor sleep, irritability) may opt for hormone replacement therapy (HRT) under expert guidance. When this treatment is correctly prescribed, it clearly improves quality of life. The most effective hormone to reduce symptoms is oestrogen. If the patient is only taking oestrogen, however, this will also stimulate the lining of the uterus. This can lead to blood loss and a prolonged intake of oestrogen increases the risk of uterine cancer. If progresterone is added to the oestrogen hormone, uterine bleeding and cancer is prevented. The risk of uterine cancer will be even lower than in women not taking hormones. The disadvantage of the daily combination of high-dose oestrogens and progestogens, for a period greater than five years, is the slight increase in breast cancer. Especially with synthetic hormones. This increase in breast cancer is due to the progesterone. Indeed, placebo-controlled randomized trials have shown that oestrogen alone does not raise the breast cancer risk. On the other hand, a big european study has shown that a combination of a natural oestrogen with a natural progesterone is safe, even after 10 years of intake. A progesterone containing spiral (IUD) can rest the uterus in women who take oestrogen alone. The IUD is not a high dose of progesterone circulating in the body and thus avoids the increased risk of breast cancer. This IUD can remain in the womb for five years. It can be placed at a routine consultation therefore avoiding oral progesterone. There are also recent data on the effect of other preparations on the breast which appear to be very promising. Each individual patient should contact her own doctor to arrange the optimal treatment for her.
A change of lifestyle after the menopause is also very important. Sport, moderate alcohol intake (one glass a day) and weight loss will also substantially reduce the risk of breast cancer. It is also essential to have at least one mammogram every two years, whether taking hormones or not. For further information, consult your doctor.
