Prevention
Modern medicine is increasingly transitioning towards preventive care. This shift towards prevention has also been observed in breast cancer care in recent years, particularly with the discovery of the BRCA gene. Subsequently, multiple genes and risk factors have been identified. Depending on these factors, a personalized screening strategy can be chosen. Therefore, it is crucial to understand these genetic and risk factors.
Diagnosis
I was diagnosed with cancer ... This website serves as a portal designed to assist you and your loved ones in accessing personal information and finding solutions to your concerns.
The primary goal of this website is to offer guidance and support to patients as they navigate their journey toward recovery and improved quality of life. The "Diagnosis" section of our website is divided into two main categories. Firstly, under "Anatomy and Physiology," we provide fundamental knowledge about the breast. Secondly, in the "Tumors and Disorders" section, we delve deeper into various breast-related conditions.
Moreover, we aim to provide information to women who may be concerned about potential breast issues but are hesitant to seek immediate medical advice. Knowledge and information can often offer immediate reassurance if a woman is able to identify the issue herself and determine that no specific treatment is necessary. Conversely, we also strive to educate women who have received a diagnosis of a serious breast condition, such as breast cancer, and wish to approach their doctor well-informed and prepared.
Treatment
The treatment for breast cancer should immediately include a discussion about reconstruction. Our foundation has no greater goal than to raise awareness of this among patients and oncological surgeons. By making an informed decision beforehand, we avoid closing off options for later reconstruction while still considering the oncological aspect. Of course, survival is paramount, and the decision of the oncologic surgeon will always take precedence.
The "Reconstruction or not?" page contains all the information you can expect during an initial consultation before undergoing tumor removal. This page is comprehensive, and your plastic surgeon will only provide information relevant to your situation.
"Removing the tumor" details the surgical procedure itself. This is the most crucial operation because effective tumor removal remains paramount. We guide you through the various methods of removal, a decision often made by a multidisciplinary team comprising oncologists, radiologists, pathologists, radiotherapists, breast nurses, gynecologists, oncological surgeons, and plastic surgeons.
The "Breast Reconstruction" section includes information and illustrations of the different reconstruction options along with corresponding steps.
Revalidation
Those treated for cancer often need a long period to recover.
Cancer is a radical illness with a heavy treatment. Often, people have to deal with psychosocial and/or physical problems afterwards, such as stress, anxiety, extreme fatigue, painful joints, reduced fitness, lymphedema... This can have a major impact on general well-being.
There are rehabilitation programmes offered by most hospitals. We cover some of the major topics here.
Quality of life
Quality of life is a key factor in coping with breast cancer. Therefore, it is important to find coping mechanisms that work, which will be different from patient to patient. For some, it may be finding enjoyment in activities they engaged in prior to diagnosis, taking time for appreciating life and expressing gratitude, volunteering, physical exercise... Of prime importance, studies have shown that accepting the disease as a part of one’s life is a key to effective coping, as well as focusing on mental strength to allow the patient to move on with life. In this section we are addressing some topics that patients experience during and after treatment and we are providing information to address them.
Screening and prophylaxis
Risk factors
Assigning a certain risk of breast cancer to a woman is very important for the development of a follow-up policy or in adopting a therapeutic attitude. In this sense, the discovery of the three known genes that may be associated with a greatly increased risk of breast cancer, BRCA-1, BRCA-2 and BRCA-3, has made a very important contribution in guiding women from these families.
Family History
A burdened family history is one of the strongest indicators of an increased risk of developing breast cancer. The more women who have been diagnosed with breast cancer in a family, the more closely related and the younger the age at diagnosis, the higher the risk of other women in that family developing breast cancer themselves.
We estimate that about 20 to 30% of all breast cancer patients have at least one relative with the same condition, in about 5 to 10% of all patients there is a strong genetic predisposition. The following elements determine a woman's risk of developing breast cancer herself:
the number of relatives who developed breast or ovarian cancer in her family,
the ratio of the number of affected to the number of unaffected women,
the degree of relationship between affected individuals,
the age at which breast cancer was diagnosed in her relatives,
the occurrence of breast cancer in both breasts (bilateral breast carcinoma) in a relative,
the occurrence of ovarian cancer in families and
the occurrence of breast cancer in men.
These elements form the starting point for assigning a high, moderate or slightly increased risk to patients. Based on this risk, advice is initially given on the optimal screening policy.
In addition to information about breast cancer risk, we also use family data to identify families in which it may be useful to initiate genetic testing. The criteria we use for this are shown in table 1. These criteria are used as a guideline: sometimes the research is also started in families that do not meet these criteria, if there are specific reasons for this. These could be, for example: a family tree that is difficult to assess (because of a small family or because there are many male relatives) or if genetic testing has important clinical implications. An exception is sometimes also made for patients with greatly increased anxiety.
Table 1. Inclusion criteria for molecular genetic research of BRCA1 and BRCA2, as they are usually used:
families with three first-degree relatives * with breast and / or ovarian cancer
families with at least two first and / or second degree relatives ** with breast and / or ovarian cancer diagnosed at a mean age below 50 years.
all patients who developed breast and / or ovarian cancer before the age of 35 years.
persons who have shown a mutation in the family.
male patients with breast carcinoma.
* first-degree relatives: mother and daughter, sisters
** second-degree relatives: grandmother and grandchild, aunt and niece
The distinction between hereditary and familial breast carcinoma cannot be made clear. The contribution of genetic abnormalities should probably be considered as a kind of continuum: in familial breast cancer, genetic abnormalities are more likely to play a role that discretely affect the risk of breast carcinoma, while in monogenic forms BRCA1 and BRCA2 mutations are present in the majority of families that increase the risk. strongly influence, see Figure 1. However, a large number of families are located on the border between both entities, in others we can detect BRCA1 or BRCA2 mutations.
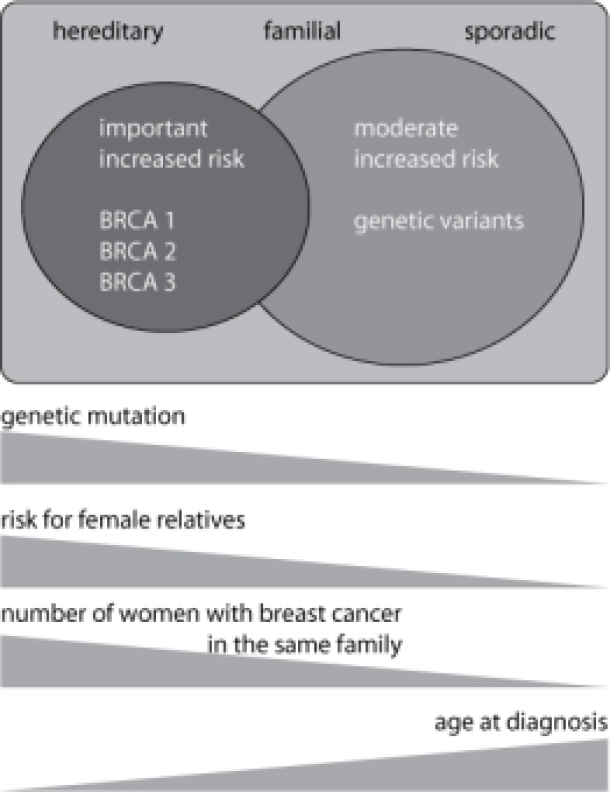
Figure: Breast cancer and its family history allow patients to be divided into three overlapping classes: the sporadic, familial and hereditary forms. Genetic abnormalities (mutations in BRCA1 and BRCA2) can most frequently be demonstrated in the hereditary form. These genetic abnormalities cause a greatly increased risk of breast and ovarian cancer in female carriers. In familial breast cancer, genetic variants probably play a role that less strongly influences the risk. The younger the age at diagnosis and the higher the number of affected relatives in a family, the greater the chance of a hereditary form. This also means that the risk of other women in the family of developing breast cancer themselves also rises sharply.
Breast density
The density of the breast tissue can be objectified on mammography. The denser the breast tissue, the higher the risk of breast cancer. Increased breast density is often a hereditary factor, but also occurs in nulliparous women (women who did not have children), women who had a first pregnancy at a later age and women who drink a lot of alcohol.
Estrogens
Estrogen plays a vital role in breast cancer development. Women whose menarche (time of first menstruation) occurs early, before 11 years of age, have an increased risk of developing breast cancer. The same is true for women with late menopause. The reverse is also true. Women who have an early menopause have a lower risk of developing breast cancer. After ovariectomy, the risk of breast cancer can even be reduced by 75% (depending on age, weight and parity).
Hormone replacement during menopause
Women with menopausal complaints (hot flushes, sweating, poor sleep, irritability) can opt to take hormones. Taking hormones requires expert guidance. When properly prescribed, this treatment will significantly improve quality of life. The most effective hormone to treat these complaints is estrogen. However, if you only take the estrogen, this will also stimulate the inner wall of the uterus. This can lead to blood loss and, if taken for a long time, to an increased risk of uterine cancer. If you add a progestant hormone to the estrogen, you can completely avoid uterine bleeding and uterine cancer. The risk of uterine cancer is then even lower than in women who do not take hormones. The disadvantage of combining high-dose estrogens and progestins on a daily basis, for a period longer than five years, is that there is a slight increase in breast cancer. This mainly occurs when taking synthetic hormones. This increase in breast cancer is due to the progestin. Indeed, placebo-controlled randomized studies show that estrogens alone do not increase the risk of breast cancer. On the other hand, large European studies show that a combination of natural estrogen with a natural progestative is safe for the breast, even after ten years of intake. Another way to avoid the intake of a synthetic progestin is to use a hormone coil. With a progestin containing coil, one can completely relax the inner lining of the uterus in women who take "estrogens alone". This IUD can remain in place in the uterus for five years. It can be placed on a routine consultation. Thus it is avoided that the progestin has to be taken by mouth. As a result, a high dose of progestin is no longer released in the body and the increased risk of breast cancer is immediately avoided. There are also recent data on the influence of other preparations on the breast. These seem to be very promising. It is therefore important to contact your doctor to individually choose the right treatment for each woman.
Obesity
The risk of breast cancer is higher in obese women (BMI> 30), especially after menopause.
Alcohol consumption
Drinking alcohol increases the risk of breast cancer. The risk increases as the number of drinks increases.
Screening
Screening helps detect new or recurring cancers at an early stage. Since both male and female carriers of genetic mutations have a high risk of tumor formation, they may wish to undergo routine screening. If a cancer is diagnosed early, the likelihood of locoregional or distant metastases is very low. Complete removal of the tumor increases the chance of a cure. However, intensive screening does not prevent cancer. The first step is regular, routine clinical examination by your doctor. A second step is additional imaging such as ultrasound, mammography and MRI.
The next consideration is the prophylactic removal of tissues in which the tumor may occur. For patients with high penetrance genetic mutations, this involves surgical removal of the breasts (bilateral skin-sparing mastectomy) and both ovaries (salpingo-ovariectomy). Just removing the ovaries reduces circulating levels of female hormones that can lead to breast cancer and stimulate breast cancer, reducing incidence by about 50%.
Although these surgical procedures are quite aggressive, they have been shown to significantly reduce the risk of cancer formation. Patients should know that nothing completely eliminates the risk. This explains why patients undergoing prophylactic surgery should still attend regular post-operative follow-up appointments.
Options available for high risk patients | ||
Breast cancer | Screening | Monthly self-examination starting at an early age > 20 yrs.: clinical examination by a physician every 3 to 6 months > 25 yrs.: yearly ultrasound & mammography, consider MRI |
| Prophylactic surgery | Prophylactic mastectomy |
| Chemoprophylaxis | Tamoxifen, especially for women previously diagnosed with breast cancer |
Ovary cancer | Screening | > 35 yrs.: gynecological examination every 6 months in combination with a trans-vaginal ultrasound & CA-125 tumor marker level |
| Prophylactic surgery | Prophylactic bilateral salpingo-oophorectomy |
| Chemoprophylaxis | None available (the possible protective effect of hormonal contraceptives is unclear) |
Male patients |
|
|
Breast cancer | Screening | No uniform guidelines |
Bowel cancer | Screening | >50 yrs.: colonoscopy |
Prostate cancer | Screening | >40 yrs.: rectal examination combined with ultrasound & PSA level |
Melanoma | Screening | Annual complete skin examination (only for BRCA-2 carriers) |
The final measure to reduce the risk of cancer formation or recurrence is chemoprophylaxis, although at this point in time, there is no scientific study that has shown any benefit in carriers of the BRCA-1, 2 or 3 mutations and therefore this option is still controversial. Only woman who have already been treated for breast cancer, which is oestrogen and progesterone receptor positive, can reduce their risk of recurrence by taking Tamoxifen. It remains to be seen whether chemoprophylaxis will be beneficial for asymptomatic carriers of genetic mutations.
Choosing between these prophylactic measures is a complex process involving both medical advice and personal choice. Important concerns for patients include: the constant worry of developing cancer, the desire to have children, femininity, inter-personal relationships, sexuality and any previous family experience with the diagnosis or treatment of cancer.
Choice is also complicated by the number of medical options for which clear benefit has not yet been demonstrated: the optimal frequency and interval of screening visits is unknown and although magnetic resonance imaging (MRI) can detect breast cancer at an earlier stage, its use in carriers of genetic mutations is still unclear.
Physicians do not have any long-term data on the impact of screening or of the more invasive options: our experience with prophylactic mastectomy is relatively short. Another area that is not clear is the benefit of hormonal substitution after bilateral oophorectomy. Scientific data has shown that administrating low-dose hormone replacement is safe but the long-term effects are still unknown.
When all the options are considered, there is no one solution that fits every patient. It is important to decide on the pathway that best suits you. Of equal importance is that each and every individual feels safe and secure with their decision, when all the potential risks have been explained. This will ultimately give peace of mind. Some women find prophylactic surgery the best solution to deal with their risk of breast or ovarian cancer while others may prefer regular screening.
Exchanging experiences with fellow patients is known to be very helpful in the decision making process. Many support groups have arisen over the last few years. They offer substantial advice and comfort for high-risk patients and often have a close working relationship with health care providers.
For male patients and male carriers of genetic mutations, unfortunately, even less data is available. Here, the main emphasis remains on routine screening to aid the early diagnosis of bowel, prostate and skin cancer.
