Prevention
Modern medicine is increasingly transitioning towards preventive care. This shift towards prevention has also been observed in breast cancer care in recent years, particularly with the discovery of the BRCA gene. Subsequently, multiple genes and risk factors have been identified. Depending on these factors, a personalized screening strategy can be chosen. Therefore, it is crucial to understand these genetic and risk factors.
Diagnosis
I was diagnosed with cancer ... This website serves as a portal designed to assist you and your loved ones in accessing personal information and finding solutions to your concerns.
The primary goal of this website is to offer guidance and support to patients as they navigate their journey toward recovery and improved quality of life. The "Diagnosis" section of our website is divided into two main categories. Firstly, under "Anatomy and Physiology," we provide fundamental knowledge about the breast. Secondly, in the "Tumors and Disorders" section, we delve deeper into various breast-related conditions.
Moreover, we aim to provide information to women who may be concerned about potential breast issues but are hesitant to seek immediate medical advice. Knowledge and information can often offer immediate reassurance if a woman is able to identify the issue herself and determine that no specific treatment is necessary. Conversely, we also strive to educate women who have received a diagnosis of a serious breast condition, such as breast cancer, and wish to approach their doctor well-informed and prepared.
Treatment
The treatment for breast cancer should immediately include a discussion about reconstruction. Our foundation has no greater goal than to raise awareness of this among patients and oncological surgeons. By making an informed decision beforehand, we avoid closing off options for later reconstruction while still considering the oncological aspect. Of course, survival is paramount, and the decision of the oncologic surgeon will always take precedence.
The "Reconstruction or not?" page contains all the information you can expect during an initial consultation before undergoing tumor removal. This page is comprehensive, and your plastic surgeon will only provide information relevant to your situation.
"Removing the tumor" details the surgical procedure itself. This is the most crucial operation because effective tumor removal remains paramount. We guide you through the various methods of removal, a decision often made by a multidisciplinary team comprising oncologists, radiologists, pathologists, radiotherapists, breast nurses, gynecologists, oncological surgeons, and plastic surgeons.
The "Breast Reconstruction" section includes information and illustrations of the different reconstruction options along with corresponding steps.
Revalidation
Those treated for cancer often need a long period to recover.
Cancer is a radical illness with a heavy treatment. Often, people have to deal with psychosocial and/or physical problems afterwards, such as stress, anxiety, extreme fatigue, painful joints, reduced fitness, lymphedema... This can have a major impact on general well-being.
There are rehabilitation programmes offered by most hospitals. We cover some of the major topics here.
Quality of life
Quality of life is a key factor in coping with breast cancer. Therefore, it is important to find coping mechanisms that work, which will be different from patient to patient. For some, it may be finding enjoyment in activities they engaged in prior to diagnosis, taking time for appreciating life and expressing gratitude, volunteering, physical exercise... Of prime importance, studies have shown that accepting the disease as a part of one’s life is a key to effective coping, as well as focusing on mental strength to allow the patient to move on with life. In this section we are addressing some topics that patients experience during and after treatment and we are providing information to address them.
Sentinel node biopsy
During surgery for removal of a malignant breast tumor, it is also possible to evaluate the axillary lymph nodes for the presence or absence of loco-regional metastasis from the breast. The aim of this procedure is to determine the severity and extent of the disease. Based on the involvement of axillary nodes, additional (adjuvant) therapies will be arranged, including chemotherapy, radiotherapy, immunotherapy and / or hormonal therapy. If large or invasive tumors or multiple small invasive breast tumors are present, all the nodes in the lower part of the axilla are removed.
Previously, more aggressive surgery was undertaken i.e. removal of all the lymph nodes around the blood vessels and nerves of the arm and behind the clavicle (axillary clearance) but this appeared only to cause more complications without giving any additional information.
The major complications were lymphedema and chronic nerve pain in the arm. Lymphedema (inability to drain lymphatic fluid resulting in its accumulation in the affected limb) is still the most frequent complication of axillary surgery but is less frequent with more conservative measures. The risk of lymphedema is increased when radiation is administered to the axilla.
When the tumor is less than 2 cm, a sentinel node biopsy is performed. Before surgery, a mildly radioactive substance is injected around the tumor. This substance moves through the lymph vessels to the axillary nodes. The first axillary lymph node reached by the fluid, the sentinel node, is the most radioactive one (fig. 1). If malignant cells from the breast tumor pass into the lymphatic vessels then the sentinel node will be the first node involved.
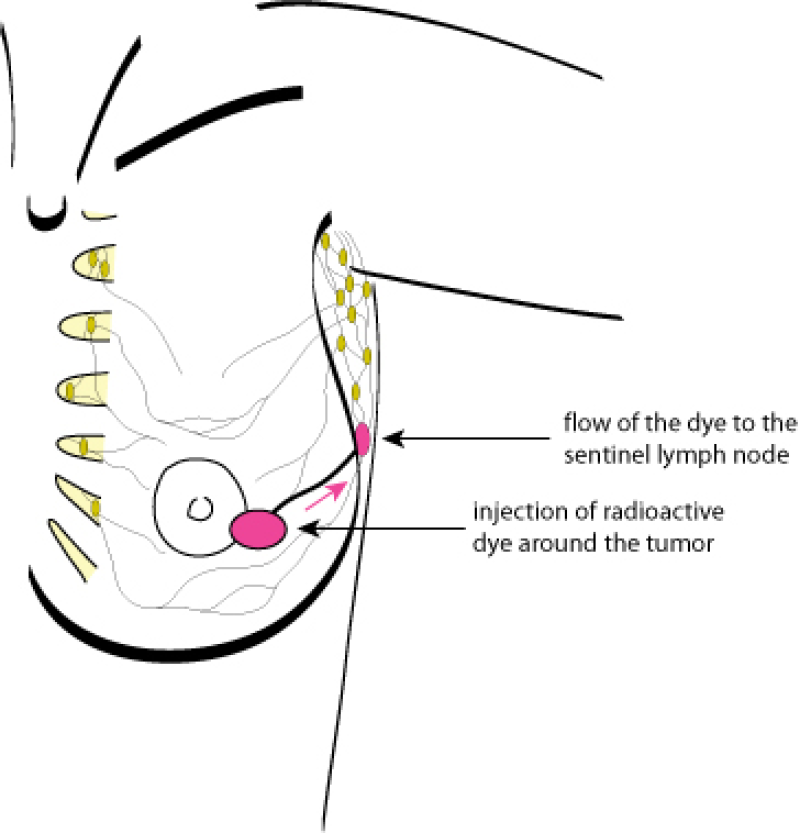
Figure 1: identification of the sentinel lymph node
During surgery, a sensitive device (Geiger counter) that measures radioactivity, is used to detect the sentinel node. This is then excised and sent for histological examination. If the sentinel node is free of malignant cells, it is not necessary to remove the other lymph nodes in the axilla. A sentinel node biopsy is a minimally invasive, short procedure. Side effects, including the risk of lymphedema, are minimal.
If the sentinel node is invaded by malignant cells, a conventional removal or “clearance” of the lower part of the axillary lymph nodes is performed in an additional surgical procedure (fig. 2).
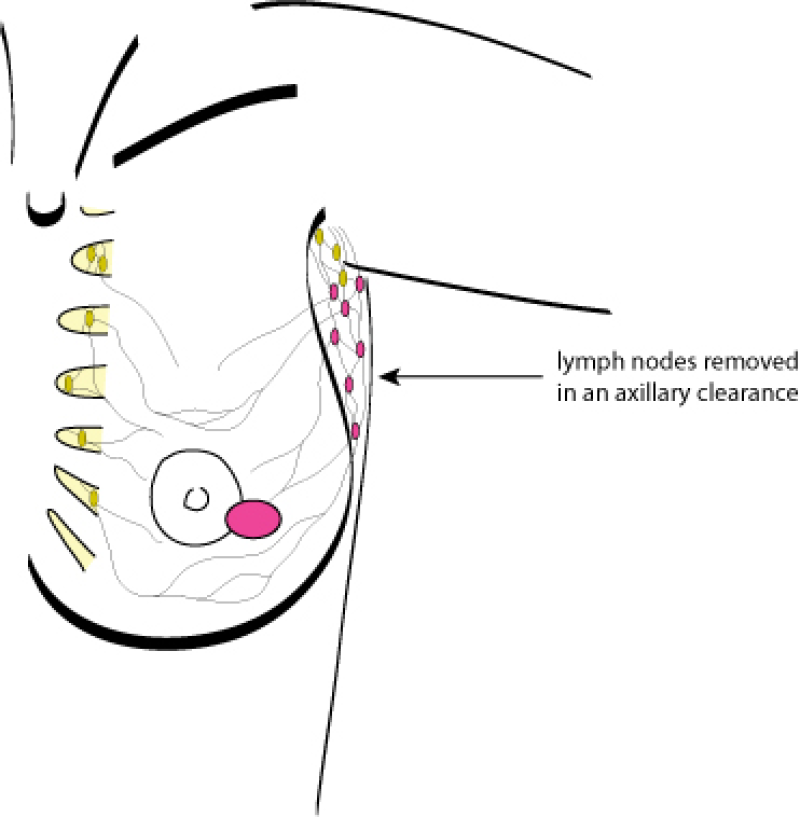
Figure 2: axillary lymph node removal
